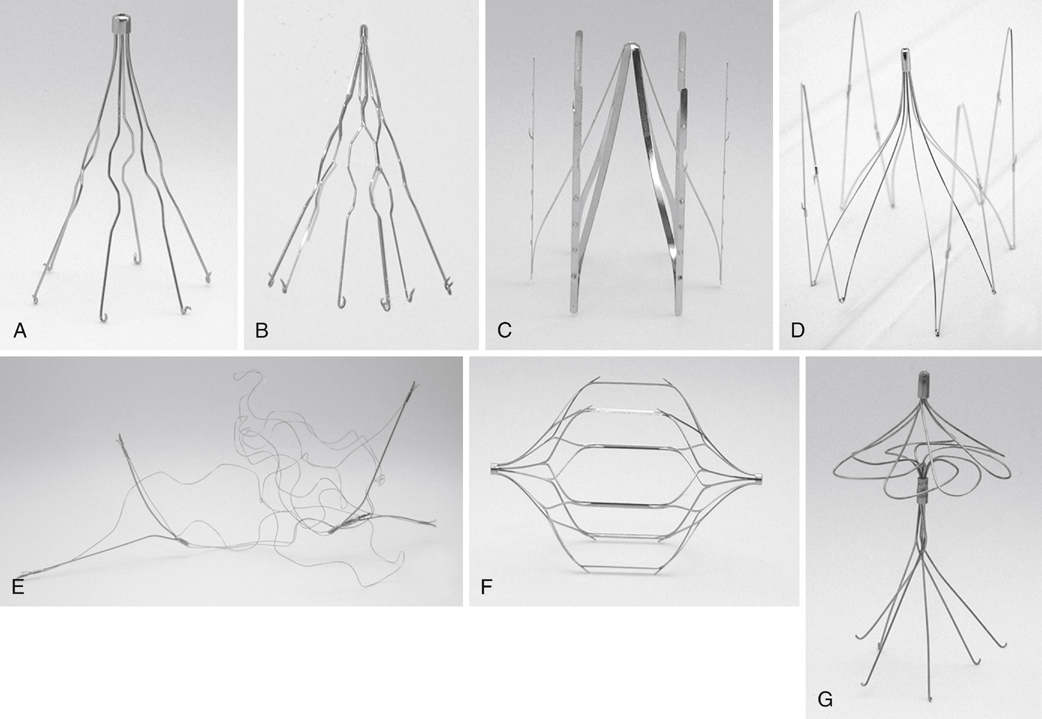
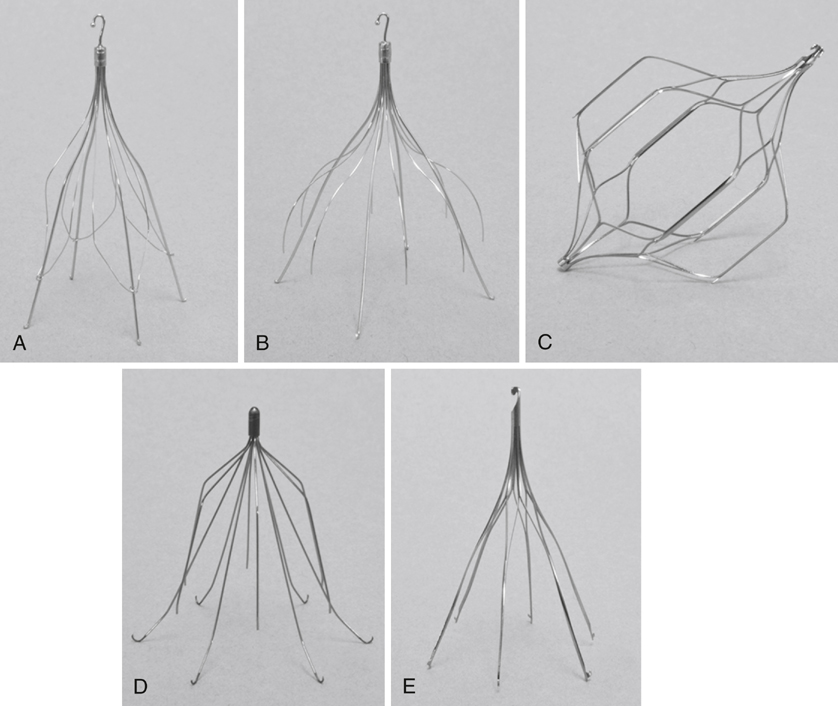
Since the advent of the first modern IVC filter by Greenfield in 1972, additional IVC filters have been developed. Many of these filters have deviated from the traditional conical design. They differ in the number of levels of filtration and the material used for construction. Currently, 13 IVC filters are approved by the U.S. Food and Drug Administration (FDA) for use in the United States. Seven of these filters are permanent: the Greenfield stainless steel filter and titanium filter (Boston Scientific), the VenaTech LGM and LP filters (B Braun), the Gianturco–Roehm Bird’s Nest filter (Cook), the TrapEase filter (Cordis), and the Simon nitinol filter (Bard) (Figure 1). The other six are retrievable filters: the Celect and Günther Tulip filters (Cook); the OptEase filter (Cordis); the Recovery nitinol, G2, G2 X, Eclipse, and Meridian filters (Bard); and the Option filter (Argon) (Figure 2). These filters are specifically designed with hooks or other features that allow recapture and removal of the filter. These filters also tend to be designed to be reconstrained and are constructed of nitinol or similar materials. All retrievable filters in the United States currently approved by the FDA are also approved for permanent placement.
The rationale for retrieval filters is largely the result of a single prospective randomized trial. The PREPIC (Prévention du Risque d’Embolie Pulmonaire par Interruption Cave) study is the only long-term randomized study comparing IVC filter placement to anticoagulation alone for preventing PE. This study’s initial 2-year results were published in 1998. In this multi-institutional trial, 400 patients with venographically confirmed acute proximal DVT were randomized to treatment with anticoagulation alone versus anticoagulation and a permanent caval filter. At 12 days, there were two PEs in the filter group (1.1%) versus nine PEs in the nonfilter group (4% vs. 8%, p = .03). At 2 years, there were six PEs in the filter group (3.4%) and 12 PEs in the nonfilter group (6.3%) (p = .16). The incidence of recurrent DVT was 37 (20.8%) in the filter group and 21 (11.6%) in the nonfilter group (p = .02). These 2-year results suggest that caval filters provided significant additional short-term protection from PE compared with anticoagulation and that this benefit seemed to wane over time and was associated with an increased risk of recurrent DVT.
The 8-year results of the PREPIC trial, published in 2005, showed that there were nine PEs in the filter group (6.2%) versus 24 PEs in the nonfilter group (15.1%) (p = .08). The filter group had 57 patients with DVT (35.7%) versus 41 (27.5%) in the nonfilter group (p = .042). The incidence of postthrombotic syndrome was similar (70.3% in filter patients vs. 69.7% in nonfilter patients) at 8 years. Mortality was also similar (103 filter vs. 98 nonfilter patients). These results suggest that at 8 years, vena cava filters reduced the risk of PE while somehow increasing the incidence of DVT and that they had no effect on the incidence of postthrombotic syndrome or on survival.
Unfortunately, several concerns have been raised regarding the PREPIC study design and analysis. Although the study has been heralded as a study of filter randomization in patients with DVT, it actually contained a study arm in which patients were randomized to treatment to unfractionated and low-molecular-weight heparins. Many argue that the PREPIC study was underpowered for such a design and that the statistical analysis did not take into account the multiple comparisons. Additionally, the lack of standardization in the types of filters used in the study has also been greatly criticized. Others point out that the finding that permanent IVC filter placement protected against PE in the long term was underemphasized in reporting study results.
Additional arguments for developing retrievable filters included concerns about leaving IVC filters in young trauma or orthopedic patients because their time at risk for VTE is limited and they have long life expectancies. Although rather rare, long-term IVC filters can result in penetration of the IVC, perforation of surrounding structures, embolization, or thrombosis of the IVC itself.