Peripheral Vascular Occlusive Disease—Rest Pain/Ulcers
HUITING CHEN and KATHERINE GALLAGHER
Adapted from a previous version by Leslie D. Cunningham and Michael S. Conte
Presentation
An 88-year-old man with a history of diabetes, congestive heart failure (CHF), hypertension, and hypercholesterolemia, status post three-vessel coronary artery bypass graft (CABG) × 10 years ago, presents to the clinic with 6 months of worsening left foot pain that localized to the forefoot. The pain is present at rest, improves with dependency, and worsens when lying in bed or with foot elevation. He has never had deep venous thrombosis. He lives alone and walks small distances around the house. On examination, he has no carotid or abdominal bruits and no palpable abdominal masses. His femoral pulses are easily palpable and equal. He has no other palpable pulses below this level on the left, but has a palpable right popliteal pulse. Biphasic Doppler signals are insonated in both the dorsalis pedis and posterior tibial arteries (DPA and PTA, respectively) on the right, and a monophasic signal is appreciated in the DPA and PTA on the left. His left foot demonstrates rubor when dependent and pallor on elevation. There is a marked absence of hair on the leg, and the skin appears atrophic, dry, and scaly. Of note, there are vein harvest incisions on the bilateral medial thighs.
Differential Diagnosis
The differential diagnosis of ischemic rest pain includes the pain and paresthesias of diabetic peripheral neuropathy, gout, rheumatologic disorders, osteoarthritis, and common foot conditions such as plantar fasciitis, bone spurs, and benign muscle cramps. The influence of dependency and elevation on this patient’s foot pain and color are nearly pathognomonic of severe chronic ischemia and would not be typical of these other conditions. Ischemic rest pain is typically localized to the forefoot (toes, instep) and is usually severe enough to require narcotics for adequate management. Benign nocturnal muscle cramps in the calf or thigh are a common condition not associated with circulatory disease. Trophic changes of the skin and loss of dermal appendages over the leg and foot are characteristic of chronic ischemia. In this setting, it is important to examine the feet for ulcers that occur at points of friction. A history of poor healing or infection that leads to amputation following minor trauma is also suggestive of severe ischemia or poorly controlled diabetes.
Background and Workup
Background
Atherosclerosis is a systemic disease. This obligates one to assess other vascular beds (cerebral, coronary, mesenteric, renal, and aortoiliac) for ischemic symptoms when evaluating a patient for complaints of infrainguinal arterial insufficiency. Recognized risk factors for atherosclerosis include tobacco use, male gender, diabetes, hyperlipidemia, hypercholesterolemia, and hypertension. Patients initially presenting with calf claudication are at increased risk for cardiovascular death, but at relatively low risk for limb loss (approximately 5% and 1% per year, respectively). In contrast to patients with claudication, reported 5-year mortality rates for patients with critical limb ischemia (critical limb ischemia (CLI); rest pain or gangrene) range from 30% to almost 90%. Factors associated with higher mortality rates are diabetes, renal insufficiency, and renal failure. The goal of revascularization procedures in this patient population is limb salvage of inpatients with rest pain; approximately 75% will achieve relief from treatment of inflow disease alone. This is in contrast to patients with tissue loss who often require treatment of inflow and outflow disease.
Initial objective testing for lower limb ischemia is done in the noninvasive vascular laboratory. Studies performed include an ankle-brachial systolic pressure index (ABI), segmental Doppler pressure (SDP) measurements, and pulse volume recordings (PVRs). These are helpful in distinguishing ischemic pain from other causes of limb pain and aid in the assessment of the level (aortoiliac vs. femoropopliteal vs. tibial) and severity of the occlusive disease. The ABI is a ratio of ankle systolic pressure to the higher brachial artery pressure and is easily performed in the clinic or at the bedside with the use of a handheld Doppler. An index of less than 0.7 variably correlates with symptoms of calf claudication. An ABI of less than 0.4 is often associated with a history of rest pain or ulcer on physical examination. In diabetic or renal failure patients, TBI values should be performed as ABIs are often invalid due to severe calcification.
SDP measurements assess the drop-off in systolic blood pressure due to occlusive disease. These are measured by inflating blood pressure cuffs at several locations along the length of the leg. The systolic pressure at which a continuous wave Doppler signal insonated at the ankle returns is compared to the higher of the brachial artery pressures measured. The difference in the pressures measured is attributable to occlusive disease proximal to the blood pressure cuff. Pressure drops of greater than 20 mm Hg are generally considered physiologically significant. PVRs are obtained with blood pressure cuffs inflated to 60 to 70 mm Hg placed along the leg in locations similar to SDP measurements. These partially inflated cuffs transmit changes in leg volume that occur with cardiac systole. The waveforms obtained indirectly correlate to the arterial pressure waves generated by the heart during systole. Damping (decrease) of the waveform is related to the presence and severity of occlusive disease proximal to the measuring cuff. PVRs are particularly useful in settings where cuff measurements of systolic pressure may be artificially elevated by arterial calcification.
Workup
This patient will require noninvasive arterial testing and an angiogram to assess for outflow disease. Since this patient has palpable femoral pulses, we prefer angiogram over CTA to evaluate outflow disease.
Noninvasive Laboratory Workup
The patient has an ABI of 0.22 and a severely depressed waveform of the PVR at the metatarsal level on the left, consistent with critical ischemia of the left foot. On angiogram, there is significant arterial occlusive disease in the superficial femoral/popliteal artery and tibioperoneal system. Additionally, the superficial venous duplex confirms that the GSV bilaterally has been harvested and that the cephalic and small saphenous veins bilaterally are under 2 mm in diameter.
Arteriogram Report
There is no significant stenosis of the distal aorta, left common iliac artery, or external iliac artery (not shown). There is mild stenosis of the left common femoral artery (CFA). Arteriogram shows a patent CFA, occluded superficial femoral artery (SFA), and a patent profunda femoris artery (PFA) (Fig. 1). The left SFA is occluded at its origin and reconstitutes at the level of the tibialis. The posterior tibial (PT) and peroneal (PE) artery are the major runoffs to the foot (Fig. 2).
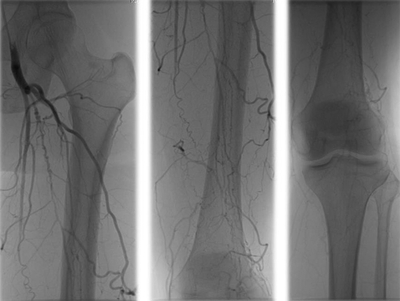
FIGURE 1 Extremity angiograms demonstrating: left patent common femoral artery, occluded superficial femoray artery (SFA), and a patent profunda femoris. Multiple collaterals visualized along the length of the occluded SFA.



