Fig. 25.1
Sharp laceration due to glass to the ulnar nerve
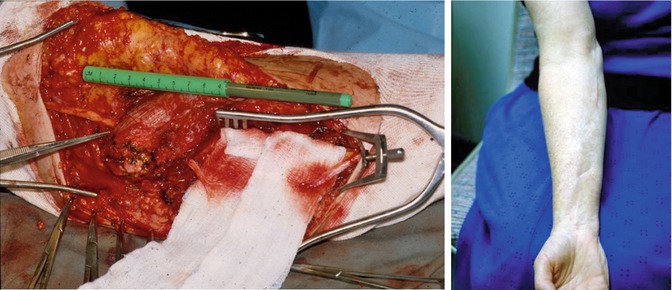
Fig. 25.2
Blunt laceration due to chain saw to the median nerve
25.3.2 Lesions in Continuity
The most severe nerve injuries do not transect or distract nerves but leave them in gross continuity. Lesions in continuity can be either focal or diffuse and may even have skipped areas of damage, depending on the mechanism of injury. In most cases, the entire cross section of the nerve has a similar extent of internal damage [28]. In some cases, one or more fascicles may be partially or completely spared, with clinic examination showing partial neurological deficits. Effective spontaneous regeneration depends on minimal connective tissue damage. Predicting which lesions in continuity will recover adequate distal function spontaneously is difficult; however, the mechanism of injury can help determine this. A less severe compressive or contusive injury, a very mild stretch injury, or a gunshot wound (GSW) is more likely to spare some internal connective tissue architecture and permit a structured axonal regenerative response. Those injuries resulting from more contusive and stretching forces associated with high-speed land, water, and air accidents are less likely to regenerate in a fashion leading to useful distal function. Despite these generalizations, it is difficult to predict outcome; therefore, most lesions of continuity are followed clinically and reevaluated at intervals for several months before surgical repair is undertaken [25, 29].
25.3.3 Stretch, Traction, and Contusion
Blunt forces imparted to nerves remain by far the most common mechanisms underlying nerve injury [30]. Normally, the nerve can withstand moderate stretch forces given its elastin and collagen-rich perineurial layer, which endows tensile strength, and its excellent ability to glide during physiologic motion [31]. Even an 8 % stretch can lead to a disturbance in intraneural circulation and blood-nerve barrier function, while stretch beyond 10–20 % results in structural failure [32, 33]. Such forces can occasionally distract a nerve, pulling it totally apart or more commonly leaving it in continuity but with considerable internal damage. If distracted by substantial forces, the nerve is frayed, and both stumps are damaged over many centimeters. Retraction and scar around both stumps are severe. Mechanisms responsible for a relatively mild degree of stretch may be associated with fractures or to a lesser degree from surgical retraction [34]. More commonly, traction forces are sufficient to tear apart intraneural connective tissue structure as well as disconnect axons [35]. The stretch mechanism is also responsible for segments of damage to a nerve displaced by high-velocity missiles, especially with GSWs [36].
Brachial plexus injury is a common disorder resulting from a stretch mechanism. Stretch or traction injuries to the plexus most commonly result from extremes of movement at the shoulder joint, with or without actual dislocation or fracture of the humerus or clavicle. Typically, either upper or lower elements of the plexus may suffer the predominant injury; however, with severe traction forces, all elements may be involved in addition to the phrenic nerve and even subclavian vessels. The stretched elements may be left in continuity and have a mixture of neurapraxia and axonotmesis. Most traction injuries do not cause avulsion but cause a severe degree of internal disruption. Traction along the axis of the brachial plexus can tear their roots out of the spinal cord. Other common injuries occur during the birth process, such as Erb’s palsy, which involves the upper and middle trunk from forcible depression of the shoulder. Klumpke paralysis involves damage to the lower trunk, roots, or spinal nerves from hyperabduction of the arm. The important point with stretch injuries is that although some may improve, many do not require operative reconstruction [1].
25.3.4 Gunshot Wounds
A frequent source of contusion and stretch injury to nerves are GSWs. In the majority of cases, nerves injured by GSWs are left in physical continuity (Fig. 25.3) [37]. In 85 % of missile injuries, there is not a direct strike to the nerve, but nerve injury may be as severe as in a direct hit [38]. As the missile approaches the nerve, the nerve explodes away from its trajectory and then implodes back as the missile passes by [39]. These dual acute stretching forces as well as contusive forces can result in a neurapraxic block in conduction, axonotmesis, neurotmesis, or a mixture. If missiles transect or partially lacerate a nerve, the lesion is a blunt and not a sharp injury. The nerve end tends to be shredded and irregular, with hemorrhagic contusive changes in both stumps [40]. Subsequently, a bulbous proximal neuroma and less-swollen distal neuroma form as with other blunt transecting mechanisms like fan blades, propellers, and chain saws. Because it takes time to determine the extent of tissue damage, a delay in exploration and repair is usually indicated [41].
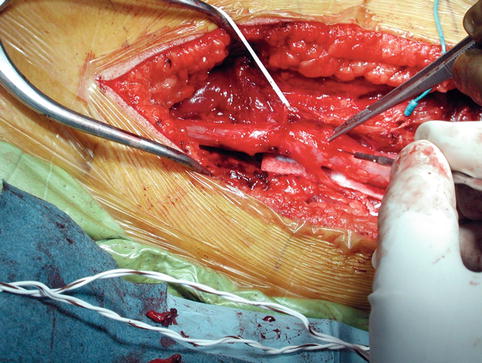
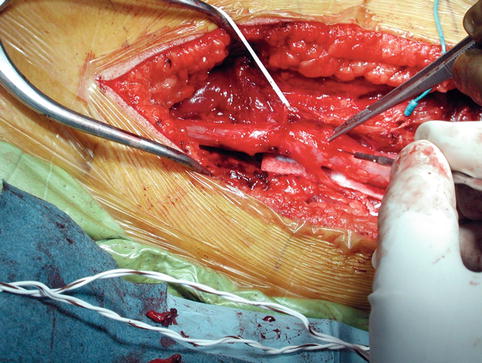
Fig. 25.3
Sciatic nerve injury by gunshot wound
25.3.5 Compression
Compression of nerve fibers appears to produce alterations in paranodal myelination, axonal thinning, and segmental demyelination. The degree of recovery after compression or ischemic injury may be accurately predicted in some clinical situations. Most palsies associated with unconsciousness due to anesthesia or poor positioning or pressure during operations as well as those related to improper application of plaster casts carry a good prognosis for spontaneous recovery [42]. Sometimes the compression or crushing injury has been severe or prolonged enough to cause damage that is irreversible unless an operative procedure is done. The brachial plexus, ulnar, sciatic, and peroneal nerves are the most commonly affected.
25.3.6 Compartment Syndrome
Volkmann contracture, a serious complication of undetected compartment syndrome, can occur from severe swelling and hemorrhage into the anterior compartment of the forearm or prolonged ischemia from brachial artery injury, which results in diffuse segmental damage to the median nerve and volar forearm muscles [43]. This type of ischemia is frequently associated with supracondylar fracture of the humerus and dislocation of the elbow; however, blunt trauma can result in enough swelling to compress nerves. Ischemia of a sufficient magnitude to produce Volkmann’s contracture results in severe endoneurial scarring over so long a segment of the median nerve that spontaneous regeneration is unlikely. In addition to the median nerve, the radial and even occasionally the ulnar nerve may be involved because of a severely swollen elbow and forearm. Compression of the median nerve must be immediately relieved by operation. Similarly, anterior compartment syndrome of the leg results in progressive peroneal palsy or foot drop, often from a fracture of the tibia or fibula. Compartment pressures can be directly measured if needed, as is discussed elsewhere. If the difference between arterial pressure and tissue pressure is less than 40 mmHg, or the compartment pressure is greater than 30 mmHg, ischemic infarction is likely to occur.
25.3.7 Electrical and Thermal Injury
Electrical injury by passage of a large current through a peripheral nerve usually results from accidental contact of the extremity with a high-tension wire [44]. Conservative management of the nerve injury with early orthopedic reconstruction seems to have the best outcome [45]. Prognosis with low-voltage injuries is excellent but variable with high-voltage injuries [45]. Histologically, electrical injury causes necrosis with subsequent replacement with connective tissue. Though uncommon, thermal injury can result in neural damage from a transient neurapraxia to severe neurotmesis with extensive necrosis. Direct injury or secondary damage from constrictive fibrosis can affect long lengths of nerves, often necessitating nerve grafts.
25.4 Clinical Evaluation and Testing
Detailed history and thorough physical examination are essential for evaluation of nerve injuries. Before a lesion to a peripheral nerve can be ruled out, it is necessary to assess that the most distal portion of that nerve is functioning [46, 47]. For the upper limb, gross innervation can be confirmed by having the patient make a five-fingered cone with the tips of the fingers and then extending the thumb [48, 49]. The intact ulnar nerve bunches the fingers into a cone and the opponens pollicis muscle, which is innervated by the median nerve, brings the thumb to the fingers. The radial nerve extends the thumb. Similarly for the lower extremity, if the great toe can be extended, the peroneal nerve is intact, and if the great toe can be flexed, the tibial nerve is intact.
Sensory and autonomic function testing is equally important. The median and ulnar nerves can be tested by pinprick over the palmar surface of the distal phalanx of the index finger and little finger, respectively; however, the radial nerve has no reliable autonomous zone for testing. The tibial nerve can be tested by stimuli to the heel, and the peroneal nerve can be tested by stimuli to the dorsum of the foot in the web space of the first toe. The presence of Tinel’s sign, i.e., percussion on a distal nerve causing paresthesias, provides some evidence favoring axonal regeneration, though it does not predict the quantity or quality of the new fibers [1].
Electromyography is valuable in localizing nerve lesions. There are three phases to EMG. The first is a brief burst of electrical activity in response to needle placement in the muscle. The second is flat line reflecting the muscle at rest. The third is an electrical response to muscle contraction or nerve stimulation. With serious denervation, there is loss or severe reduction in Phase I, with spontaneous firing of rapid biphasic, low-amplitude sharp waves or fibrillations in Phase II. In Phase III there is either no evoked muscle action potential or a poorly formed one [1].
Myelography is an important test for supraclavicular brachial plexus injuries as well as lumbosacral stretch injuries [50–53]. If a meningocele is present, this suggests an avulsed nerve root or severe internal damage. Presence of a meningocele indicates that there was enough force to produce an arachnoid tear. Computed tomography (CT) scans are useful for stretch injuries, and magnetic resonance imaging (MRI) can confirm degeneration of a nerve.
25.5 Operative Care
External neurolysis involves cleaning the nerve of investing tissues, thereby freeing up the nerve in a full circumferential fashion. After neurolysis has been completed, the nerve should be assessed to determine whether further intervention is needed. Stimulating and recording electrodes are placed on the nerve proximal to the lesion, which should produce a recordable nerve action potential (NAP). The electrodes are then moved distally, and if there is a NAP below the level of intervention, this suggests that the time interval since injury is less than 9 months, making recovery likely with external neurolysis alone [1].
Internal neurolysis involves careful splitting of a nerve into its individual fascicles. An indication for internal neurolysis is an injury that is more severe to one portion of a nerve than another that requires a split or partial repair despite the presence of a transmitted NAP across the lesion. Other indications include severe neuropathic pain for which conservative medical management has failed [1].
If a nerve has been transected or if a short gap exists following the resection of a lesion in continuity, an end-to-end epineurial repair can be performed. The proximal and distal ends are debrided, the stumps are mobilized, and a tension-free repair is performed. The limb needs to be immobilized for several weeks in order to prevent any tension on the repair. At times, the length of the resected nerve is too long for direct repair and a graft is needed. Most grafts are fashioned from the sural nerve, although cutaneous nerves of the forearm can also be used [1].
Nerve transfer is the substitution of a functioning, expendable nerve or part of a nerve with a nonfunctioning nerve. Transfers are indicated for preganglionic injuries in which nerve grafting would not be possible, but with the success rate of transfers, surgeons are now using transfers rather than grafts for postganglionic injuries [1].
25.6 Brachial Plexus
The brachial plexus originates from the C5 to T1 spinal nerve roots and branches into three trunks, followed by the anterior and posterior divisions and the three cords (medial, lateral, and posterior) (Fig. 25.4). The nerves, their innervated muscles, and impact from injury are detailed in Table 25.1. Suprascapular nerve injury is common in athletes who receive repetitive trauma from shoulder depression and abduction or in stretch injuries from humeral or midshaft clavicular fractures [54].
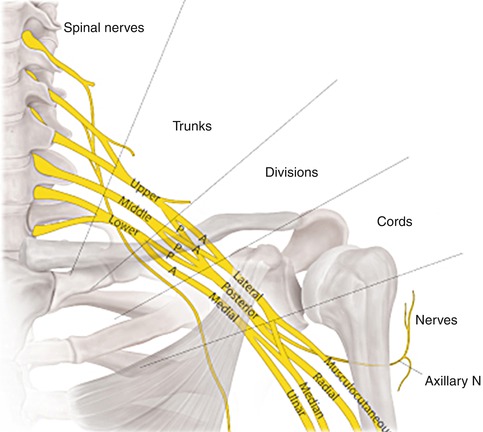
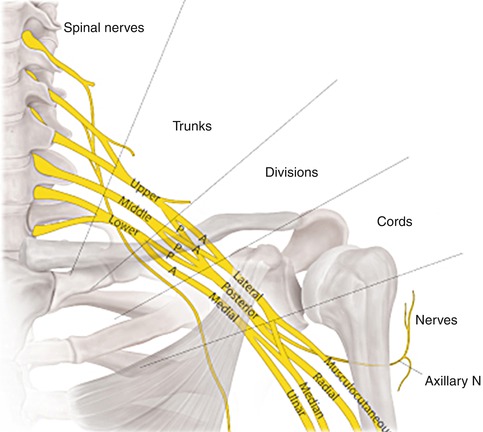
Fig. 25.4
The five regions of the brachial plexus and their relation to the anterior tubercles, clavicle, and coronoid process
Table 25.1
Nerve root and muscle innervations
Nerve | Root/origin | Muscle innervated | Result if injured |
|---|---|---|---|
Dorsal scapular | C5 | Rhomboid | Some winging of the scapula; awkward shoulder abduction |
Long thoracic | C5–7 | Serratus anterior | Severe winging of scapula |
Suprascapular | Upper trunk plexus | Supraspinatus; infraspinatus | Difficulty with initial abduction/external rotation |
Axillary | Posterior cord plexus | Deltoid | Difficulty with abduction beyond 30° |
Thoracodorsal | C6–8 | Latissimus dorsi | Difficulty with shoulder adduction |
A very proximal injury to the C5 nerve root results in paralysis of the rhomboids, deltoid, and supraspinatus and weakens the serratus anterior and infraspinatus. The biceps and brachialis may display partial weakness due to dual supply with C5 and C6. Sensory loss may also be present over the cap of the shoulder. C6 injuries may impact on biceps, brachialis, supinator, and brachioradialis, a strong flexor of the elbow. The latissimus dorsi, another adductor of the arm, is weak or paralyzed with proximal C6 lesions. With an upper trunk lesion (C5–6), the posture of the upper extremity and hand is that of Erb’s palsy, with paralysis of supraspinatus, infraspinatus, deltoid, latissimus dorsi, biceps/brachialis, brachioradialis, and supinator [1].
The middle trunk is formed by the C7 nerve root and supplies most of the triceps, which extends to the forearm. Fibers from the middle trunk may also provide input to the extensor carpi radialis and sometimes to the extensor carpi ulnaris, which dorsiflex the wrist. A proximal C7 nerve injury can result in loss of fibers to the lateral cord, which supplies the pronator teres as well as wrist and finger flexors. Isolated C7 injuries result in paresis and not paralysis as they contribute predominately to muscles supplied by one or more other roots.
The lower trunk includes the C8 and T1 nerve roots. Finger and thumb extensors as well as flexors and intrinsics primarily receive input from C8. Loss results in weakness or paralysis of extensors to the thumb, forefinger, and long finger. Sensory loss may result in ulnar distribution involving the ring and little finger. T1 supplies the hand intrinsics, especially the abductor digiti minimi and opponens digiti minimi. Sensory loss may occur with lesions here as well as in the ulnar distribution. With injury to the lower trunk, a complete loss of all hand intrinsics, including those in the ulnar and median distribution, occurs as well as variable degrees of finger and wrist flexor loss [1].
With brachial plexus injuries, electromyographic studies as well as plain radiographs can be helpful for evaluations of fractures in the area. Concomitant vascular injuries may be assessed with angiography or venography. Myelography can be helpful if nerve root avulsion is in question. CT and MRI are good studies for ruling out tumors and may be able to replace myelography and other studies in the future for determining nerve damage.
Sharp injury with laceration to the tissues surrounding the brachial plexus has the potential to transect a portion of the plexus. The presence of Tinel’s sign elicited by tapping the supraclavicular area can be quite useful in differentiating between spinal nerve transection or rupture and root avulsion [55]. A positive Tinel’s sign, which is perceived by the patient as tingling in an anesthetic arm or hand, usually indicates transection or rupture rather than avulsion. An early repair of clean stab wounds involving C5–7 can be expected to yield a return of function close to normal levels; however similar early repair to C8–T1 results in only some recovery of hand function that is far from normal. Primary repair within 72 h is advised for sharply transected plexus elements, whereas delayed repair is reserved for blunt transections or injuries in continuity [56].
The most common injury to the brachial plexus is caused by stretch/contusion, usually secondary to motor vehicle accidents [57, 58]. Regardless of the mechanism of injury, a conservative nonsurgical approach has predominated historically. C5–6 distribution stretches have a relatively low incidence of avulsion, may recover spontaneously, and may be associated with severe damage to C7. These injuries are excellent candidates for direct repair, aided by neurotization, with very good results. C5–7 distribution stretches have more roots avulsed than C5–6 stretches and spontaneous recovery occurs less often. There is a variable loss of finger and wrist movement; nonetheless, some of these lesions are candidates for direct repair with acceptable results. Although some regain usable shoulder and arm function with C5–T1 direct repair, results overall are not as good. Graft repair from a single root, often C5, is frequently augmented with neurotization. Complications from repair include risk of phrenic nerve paralysis and pneumothorax.
Gunshot wounds are the second largest mechanism of injury to the brachial plexus following stretch/contusion. GSWs most commonly cause lesions in continuity, though transection and vascular injures occur as well. The best outcomes typically occur with upper trunk and lateral and posterior cord lesions, but recovery occurs with some C7 to middle trunk and medial cord to median nerve repairs.
25.7 Radial Nerve
The radial nerve has major contributions from the C6 to C8 nerve roots and is the major outflow of the posterior cord distal to the origin of subscapular, thoracodorsal, and axillary nerves. Innervated muscles include the triceps, anconeus, brachioradialis, extensor carpi radialis longus (ECRL), extensor carpi radialis brevis (ECRB), and through its continuation, the extensor carpi ulnaris, supinator, extensor digitorum communis, extensor digiti minimi, abductor pollicis longus, extensor pollicis longus and brevis, and extensor indicis muscles. A key clinical point in assessing the level of nerve injury is whether the patient’s latissimus dorsi muscle, innervated by the thoracodorsal nerve, and the deltoid muscle, innervated by the axillary nerve, are functioning. If both are clinically active, then the lesion spares the posterior cord and involves the radial nerve more distally. Few radial nerve injuries involve the triceps as triceps innervation is very proximal. Injury to the radial nerve at the mid-arm level from a humeral fracture is the most common mechanism of injury [59, 60].
Other mechanisms of injury at this level include GSW, contusion, simple compression or stretch without fracture, injection injury, tumors, and entrapment. The hallmarks of injury at this level are loss of brachioradialis and more distal radial-innervated functions with sparing of triceps [61, 62]. This results in characteristic wrist drop and finger drop. The radial nerve can be injured more distally by accidental drug injection, distal humeral fracture, direct contusion, or GSW [60, 63]. An elbow-level radial nerve injury causes loss of function of the ECRL and ECRB muscles. These injuries are most frequently associated with penetrating wounds, fractures, or dislocations of the elbow by cyst or tumor or Volkmann ischemic contractures [64]. Posterior interosseous nerve involvement seriously affects the function of more distal muscles but spares some supination provided by the biceps and exhibits weak wrist extension. The sensory territory of the radial nerve encompasses the dorsum of the hand and some of the wrist, though it may be small even with complete nerve injury due to overlap from the median and ulnar nerves [65]. The outcome of surgical repair of the radial nerve with or without tendon transfer is considered excellent [60, 66–68]. Despite favorable outcome with proper management of radial nerve injuries, recovery of the extensor communis and extensor pollicis longus muscles is difficult to obtain. Fortunately, tendon transfer to the extensor expansion of the digits is an excellent substitute.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


