Chapter 18 Peripheral Artery Disease
Clinical Evaluation
The least often recognized of the commonly occurring manifestations of atherosclerosis is peripheral artery disease (PAD). Epidemiological studies suggest that approximately 7.1 million people in the United States have PAD.1 Among 7458 participants aged 40 years and older from the 1999 to 2004 National Health and Nutrition Examination Survey (NHANES), prevalence of PAD was 5.9%.1,2 Despite its relative frequency, predictable patient population, and prognostic implications for life and limb, many cardiovascular physicians do not undertake clinical evaluation of PAD. This chapter will focus on the history, physical examination, and diagnostic tests important to management of limb atherosclerosis.
Patient History
Diagnosis of PAD begins with clinical suspicion in the typical patient population. This includes avid questioning and seeking to elicit historical evidence of limb and systemic atherosclerosis. Clinical suspicion should be heightened in older persons, in those with coronary or cerebral atherosclerosis, and in patients with atherosclerotic risk factors such as diabetes or tobacco use, as well as renal failure (see Chapter 16). Peripheral artery disease is uncommon before the age of 40 years. In the German Epidemiological Trial on Ankle Brachial Index (getABI) of 6990 unselected patients aged 65 years or older, prevalence of PAD in men and women was 20% and 17%, respectively.3 In the PAD Awareness, Risk, and Treatment: New Resources for Survival (PARTNERS) program, a study of 6979 patients in 350 primary care practices across the United States, ankle-brachial index (ABI) screening was performed in subjects older than age 70, or older than age 50 if they were smokers or had diabetes.4 In this primary care population, 29% of those screened with an ABI met the criteria for PAD.
Despite the relative frequency of disease, diagnosis of PAD is not often considered because the majority of patients with PAD are asymptomatic. In the PARTNERS program, only 11% of PAD patients had classic symptoms.5 Similar data have been reported in other large cross-sectional studies (see Chapter 16). Even in high-risk subgroups with a higher population frequency of PAD, the diagnosis may be missed because PAD is often asymptomatic. The decision to look for PAD in the outpatient should be predicated on the pretest probability of finding it. Application of the PARTNERS criteria, for example, demonstrated the importance of risk factors in enriching the population with PAD to make ABI screening worthwhile. Thus, the presence of risk factors for atherosclerosis should lower the threshold for routine screening.
Symptoms of Peripheral Artery Disease
The most commonly ascribed symptom that develops as a result of PAD is intermittent claudication. The word claudication derives from the Latin word claudicatio, which was used to describe the limp gait of a lame horse. As defined in the Rose questionnaire,6 claudication is development of an ischemic muscular pain on exertion. The pain can be characterized as aching, burning, heaviness, feeling leaden, tightness, or cramping. Pain should originate in a muscular bed, such as the calf, thigh, hip, or buttock, and not localize to a joint. The area of the worst blood flow limitation usually subtends the site of muscular discomfort. For example, patients who develop hip or buttock discomfort with walking most likely have distal aorta or iliac artery occlusive disease, whereas patients with calf claudication likely have superficial femoral or popliteal arterial stenoses or occlusions. Reduction of muscular work on activity cessation rebalances available blood supply with muscle demand and quickly resolves the pain.
Both time of activity to pain onset and time to pain resolution should be consistent and predictable. The distance walked to the onset of leg discomfort is called the initial claudication distance, and the maximal distance the patient can walk without stopping because of leg discomfort is called the absolute claudication distance. Several classification schemes are used to categorize the severity of claudication, including the Fontaine (Table 18-1) and Rutherford classifications (Table 18-2).7 When the interview is complete, the physician should have insight into the nature of discomfort, how long it has been present, the typical duration of exercise required to cause the discomfort, and the amount of rest necessary to relieve the symptoms.
Table 18-1 Fontaine Classification
| Stage | Description |
|---|---|
| I | Asymptomatic, ABI < 0.9 |
| II | Intermittent claudication |
| III | Daily rest pain |
| IV | Focal tissue necrosis |
ABI, ankle-brachial index.
Table 18-2 Rutherford Classification
| Grade | Category | Description |
|---|---|---|
| 0 | 0 | Asymptomatic |
| I | 1 | Mild claudication |
| I | 2 | Moderate claudication |
| I | 3 | Severe claudication |
| II | 4 | Ischemic rest pain |
| III | 5 | Minor tissue loss |
| IV | 6 | Major tissue loss |
Classic symptoms of claudication do not occur in all patients with PAD, including those with functional limitations. The application of questionnaires for claudication, such as the World Health Organization (WHO)/Rose questionnaire or the Walking Impairment Questionnaire,6,8 may underestimate PAD prevalence by 50%. Data from McDermott et al. indicate that complaints other than claudication are common.9 They evaluated functional tolerance across a range of symptoms in cross-sectional analyses of patients with and without PAD.5,10 Peripheral artery disease patients demonstrated several types of leg discomfort, including leg pain at rest and with walking, pain with walking alone requiring cessation of activity, and pain patients could “walk through.” This variety of presentations would be missed with questioning only for classic symptoms. Moreover, the type of discomfort predicted function. Patients with pain at rest and with walking had worse functional capacity than those whose pain occurred with walking and stopped with walking cessation, and those who were able to “walk through” the pain. Quality of leg pain, whether it is atypical or classic, does not predict severity of reduction in limb perfusion pressure as measured by the ABI.11
Presence of intermittent claudication has important prognostic implications regarding functional capacity and mortality. Three quarters of patients with intermittent claudication will have stable symptoms over the next 10 years; approximately 25% will progress to more disabling claudication or critical limb ischemia requiring revascularization or culminating in amputation.6 Moreover, they will suffer a mortality more than twice that of the general population, approximating 30% at 5 years.12
Differential Diagnosis of Claudication
Once exercise-related discomfort has been established, several alternate vascular and nonvascular diagnoses should be considered (Box 18-1). Vascular disorders include popliteal artery entrapment (see Chapter 62), compartment syndrome, fibromuscular dysplasia, venous insufficiency (see Chapter 55), and vasculitis (see Chapters 41 through 45). Popliteal artery entrapment typically occurs in very active persons or athletes. Because of an abnormal origin of the medial (or less commonly, lateral) head of the gastrocnemius muscle, the popliteal artery may be compressed with walking and yield symptoms of claudication. Endofibrosis of the external iliac artery (EIA), a relatively rare occurrence in highly trained cyclists and other endurance athletes, may cause claudication.
![]() Box 18-1 Nonatherosclerotic Causes of Exertional Leg Pain
Box 18-1 Nonatherosclerotic Causes of Exertional Leg Pain
Fibromuscular dysplasia is a noninflammatory arterial occlusive disease that most commonly affects the renal and carotid arteries but may involve other arterial beds (see Chapter 63).13 Any of the arteries in the lower extremities may be affected, but the iliac arteries are the most common. Fibroplasias may involve the intima, media, or adventitial layer of the artery. The most common variety is medial fibroplasia. It can be diagnosed from the “string of beads” appearance on angiography and by its predilection for the nonbranching points of vessels. The etiology of fibromuscular dysplasia remains unknown.
Critical Limb Ischemia
Critical limb ischemia (CLI) is the most debilitating manifestation of PAD (Fig. 18-1). The TransAtlantic Inter-Society Consensus (TASC) Working Group estimates that the incidence of CLI is between 300 and 1000 persons per million per year.6 Across the globe, frequency of amputation varies from 28 per million people per year in Madrid to 439 amputations per million people per year among Navajo Americans.14 Prevalence of CLI was 1.2% and affected more women than men in a population study of 8000 persons between 60 and 90 years of age.15
Diabetes and smoking increase the risk of developing CLI. Diabetes is the cause of most nontraumatic lower-extremity amputations in the United States.16 Diabetes increases the risk of amputation nearly fourfold, even with similar levels of blood flow limitation as in nondiabetic patients.17 Cigarette smoking also increases the risk that PAD will progress to CLI. In a study of 343 consecutive patients with intermittent claudication, 16% of those who continued to smoke developed CLI, compared to none in those who were able to stop smoking.18 In 190 patients undergoing lower-extremity revascularization followed for 3 years, those who smoked more than 15 cigarettes a day had a 10-fold higher risk (21%) of amputation compared to those who smoked fewer than 15 cigarettes a day (2%).19 Critical limb ischemia occurs as a consequence of tissue ischemia at rest, and it manifests as foot pain, nonhealing ulcers, or tissue gangrene. The pain is often severe and unremitting and localized to the acral portion of the foot or toes, notably at the site of ulceration or gangrene. Blood flow limitation is so severe that the gravitational effects of leg position may affect symptoms. Patients commonly report that leg elevation worsens pain. This is typically worse at night when the patient is in bed and the leg, now at heart level, no longer benefits from the dependent position. Placing the foot on the floor beside the bed is a common action used by patients to reduce pain. Inability to use the leg and chronically placing the leg in a dependent position may cause peripheral edema, a finding occasionally mistaken for venous disease in these patients. With severe ischemia, any skin perturbation, including bedclothes or blankets, may cause pain; in ischemic neuropathy, this causes a lancinating pain in the foot. Other symptoms of CLI include hypesthesia, cold intolerance, muscular weakness, and joint stiffness of the affected limb. Severity of CLI is categorized in both the Fontaine and Rutherford classification schemes (see Tables 18-1 and 18-2).
Differential Diagnosis of Critical Limb Ischemia
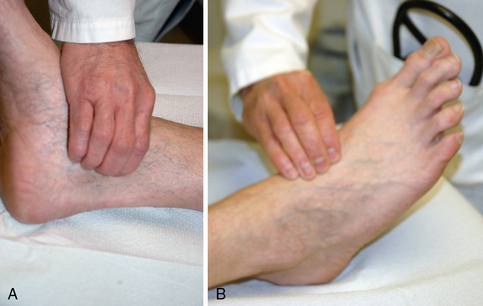
Differential diagnosis of CLI includes vascular and nonvascular diseases (Box 18-2). Atheroembolism, or blue toe syndrome, occurs when components of large-vessel atherosclerotic plaque embolize to distal vessels (Fig. 18-2) (see Chapter 47). The embolized material is composed of fibroplatelet debris and cholesterol crystals. A common cause of atheroembolism is iatrogenic disturbance of the vessel, whether from catheterization or surgery. Several features may help in differentiating atheroembolism from traditional CLI. Patients typically have pulses palpable down into the feet, because the emboli require a patent pathway to distal portions of the extremities. Other clinical clues include new renal insufficiency and blood eosinophilia. On examination, the patient will have areas of cyanosis or violaceous discoloration of the toes or portions of the feet and areas of livedo reticularis.
Acute limb ischemia may occur from thrombosis in situ or from thromboemboli of large fibroplatelet accumulations that originate in the heart or large arteries and occlude conduit arteries (see Chapter 46). These patients have an accelerated course and may present with the “five Ps” of acute ischemia: pain, pallor, poikilothermia, paresthesia, and paralysis. Other causes of limb ischemia include vasospasm, TAO, other vasculitides, and connective tissue disorders (see Chapters 41 44, and 48). Other causes of ulcers include neuropathy, venous disease, and trauma (see Chapter 61).
Nonvascular causes of foot pain include neuropathy, arthritides such as gout, fasciitis, and trauma (see Box 18-1).
Physical Examination
A comprehensive physical examination that includes general appearance of the patient, integument, heart, lungs, abdomen, and limbs should be performed during the initial patient encounter to elucidate evidence of systemic disease and provide insight into cause and manifestation of the patient’s vascular disease. The entire vascular system should be examined. Blood pressure is measured in each arm. A blood pressure difference of 10 mmHg or more may be indicative of innominate, subclavian, axillary, or brachial artery stenosis. The carotid, brachial, radial, ulnar, femoral, popliteal, dorsalis pedis, and posterior tibial pulses should be palpated in every patient (Fig. 18-3). Several pulse-descriptive schemes have been promulgated. One is to grade the pulses as 0 (absent), 1 (diminished), and 2 (normal). A very prominent or forceful pulse may occur in patients with aortic regurgitation or high cardiac output states. Absence of any pulse in the lower extremity, except in the dorsalis pedis, increases the likelihood of PAD.20 The dorsalis pedis pulse is not palpable in approximately 8% of healthy patients.20 Absence of a peripheral pulse may indicate a significant stenosis between the present and absent pulse. Occasionally, pulses may be palpable below the level of a significant stenosis. This most commonly occurs in the setting of iliac artery disease when there may be sufficient collateral vessels to maintain perfusion to distal arteries.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree