5 Peripheral Artery Disease and Peripheral Artery Angiography
Lower Extremity Peripheral Arterial Disease
PAD involving the lower extremities is diagnosed by screening studies or physical examination. Symptoms of intermittent claudication classically start distally within a muscle group (below the stenosis) and then ascend with continued activity. Rest pain that occurs with leg elevation and is paradoxically relieved by walking may suggest severe PAD (as the effects of gravity increase arterial perfusion of muscle groups). Critical PAD may present as tissue ulceration and gangrene. The American College of Cardiology/American Heart Association (ACC/AHA) has produced guidelines that suggest that individuals with PAD present in clinical practice with distinct syndromes (Table 5-1).
Table 5-1 Individuals With Peripheral Artery Disease Present in Clinical Practice with a Variety of Distinct Syndromes
| Asymptomatic: Without obvious symptomatic complaint (but usually with a functional impairment) |
| Classic claudication: Lower extremity symptoms confined to the muscles with a consistent (reproducible) onset with exercise and relief with rest |
| “Atypical” leg pain: Lower extremity discomfort that is exertional but that does not consistently resolve with rest, consistently limit exercise at a reproducible distance, or meet all “Rose questionnaire” criteria |
| Critical limb ischemia: Ischemic rest pain, nonhealing wound, or gangrene |
| Acute limb ischemia: The “five Ps,” defined by the clinical symptoms and signs that suggest potential limb jeopardy: pain, pulselessness, pallor, paresthesias, paralysis; polar as a sixth “P”) |
The physical examination is the first tool in defining the location, severity, and etiology of PAD and its symptoms. Arterial pulse intensity should be assessed and should be recorded numerically as shown in Table 5-2.
Table 5-2 Gradation of Arterial Pulse
| Numerical Gradation | Clinical Assessment |
|---|---|
| 0 | Absent |
| 1 | Diminished |
| 2 | Normal |
| 3 | Bounding |
Table 5-3 outlines some of the more important aspects of the limb examination.
Table 5-3 Physical Examination Findings of Peripheral Artery Disease
| Limb examination (and comparison with the opposite limb) includes the following: |
7. Pallor with leg elevation after 1 minute at 60 degrees (normal color should return in 10 to 15 seconds; longer than 40 seconds indicates severe ischemia) |
Noninvasive Diagnostic Testing
Measuring the ankle-brachial index (ABI) both at rest and after exercise is very useful, especially in individuals who have risk factors for PAD. Resting ABI may be insensitive for detecting mild aorto-iliac occlusive disease and is not designed to define the degree of functional limitation. However, it establishes the diagnosis of PAD and identifies a population at high risk of cardiovascular ischemic events. Incompressible arteries (elderly patients, patients with diabetes, renal failure) make such rest testing difficult. The toe-brachial index (TBI) should be used in individuals with noncompressible pedal pulses. Exercise ABI may be even more useful than resting ABI as this will “unmask” PAD when resting the ABI is normal. Performing segmental ABI and pulse volume recordings together with the ABI can indicate presence of multilevel occlusive lower extremity PAD.
Peripheral Vascular Angiography
Peripheral vascular angiography, both as a diagnostic tool and for aiding percutaneous vascular intervention, is not difficult once techniques of coronary angiography have been mastered. Angiography is usually performed after completion of noninvasive PAD screening tests (Fig 5-1).
Endovascular Percutaneous, Catheter-Based Revascularization Techniques
Endovascular reconstruction options include the following:
The efficacy of PTA versus stents for lower extremity arterial stenosis has not been demonstrated in randomized trials. PTA of distal abdominal lesions is effective; however, PTA followed by stenting offers greater advantages of larger vessel lumen gain, long-term patency (>70% at 5 years), high procedural success rates (90%), and less thromboembolism. Factors associated with a poor outcome with endovascular therapy include the following:
Iliac Artery Intervention
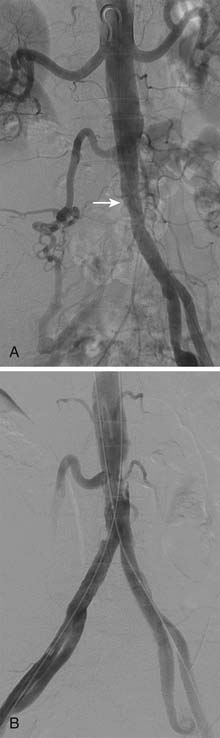
The indication to perform iliac artery intervention includes vascular access and symptomatic lower extremity ischemia. Iliac intervention may also be appropriate in patients with severe stenosis (Fig. 5-2, A and B) or occlusion of the femoropopliteal or infrapopliteal arteries and concomitant moderate iliac artery disease, in whom revascularizing the moderately stenosed iliac artery may improve the arterial inflow and lead to symptomatic improvement or salvage of the limb.
The indications for revascularization in the patient with intermittent claudication are as follows:
Femoropopliteal Artery Intervention
Atherosclerotic occlusive disease is more common in the femoropopliteal artery than in the iliac artery. When the femoropopliteal artery is involved in a symptomatic lower extremity, complete occlusions are three times more frequent than stenosis. Table 5-4 demonstrates the morphologic stratification of femoropopliteal lesions according to the Transatlantic Inter-Society Consensus (TASC). According to the TASC recommendations, endovascular therapy is the treatment of choice for type A femoropopliteal lesions and surgery is the treatment of choice for type D lesions. Endovascular treatment is the preferred treatment for type B lesions and surgery is the preferred treatment for low risk patients with type C lesions. The patient’s comorbidities, fully informed patient preference, and the local operator’s long-term success rates must be considered when making these treatment recommendations for type B and type C lesions.
Table 5-4 Morphologic Stratification of Femoropopliteal Lesions
| TASC type A femoropopliteal lesions |
| TASC type B femoropopliteal lesions • Single or multiple lesions in the absence of continuous tibial vessels to improve inflow for a distal bypass |
| TASC type C femoropopliteal lesions |
| TASC type D femoropopliteal lesions |
CFA, Common femoral artery; SFA, superficial femoral artery; TASC, Transatlantic Inter-Society Consensus.
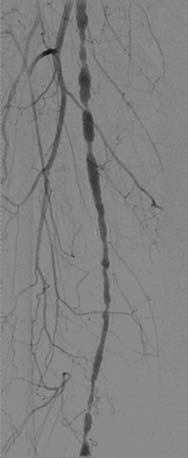
Endovascular interventions for TASC type A femoropopliteal arterial lesions have excellent procedural success and reported patency rates that vary from 30% to 80% at 1 year. The role of primary stenting for femoropopliteal disease remains incompletely defined. Stents (and other adjunctive techniques such as lasers, cutting balloons, atherectomy devices, and thermal cryoplasty devices) can be useful in the femoral, popliteal, and tibial arteries as salvage therapy for a suboptimal or failed result from balloon dilation (e.g., persistent translesional gradient, residual diameter stenosis greater than 50%, or flow-limiting dissection). The effectiveness of stents, atherectomy, cutting balloons, thermal devices, and lasers for the treatment of femoral-popliteal arterial lesions beyond this context is not well established (Figs. 5-3, 5-4, and 5-5).
Revascularization of the femoral or popliteal arteries is reserved for patients with lifestyle-limiting claudication, ischemic rest pain, and limb-threatening ischemia. Treatment of short (<5 cm) occlusions yields better results than treatment of long (>10 cm) occlusions or stenosis. The presence of patent runoff vessels correlates with long-term benefits, reflected in the improved outcome in patients with milder symptoms. Significant residual stenosis after angioplasty correlates with a poor long-term outcome, whereas the absence of diabetes correlates with an improved patency rate. Endovascular intervention is not indicated if there is no significant pressure gradient across a stenosis despite flow augmentation with vasodilators. Primary stent placement is not recommended in the femoral, popliteal, or tibial arteries (Figs. 5-6 and 5-7). Endovascular intervention is not indicated as prophylactic therapy in an asymptomatic patient with lower extremity PAD.
Vascular Access
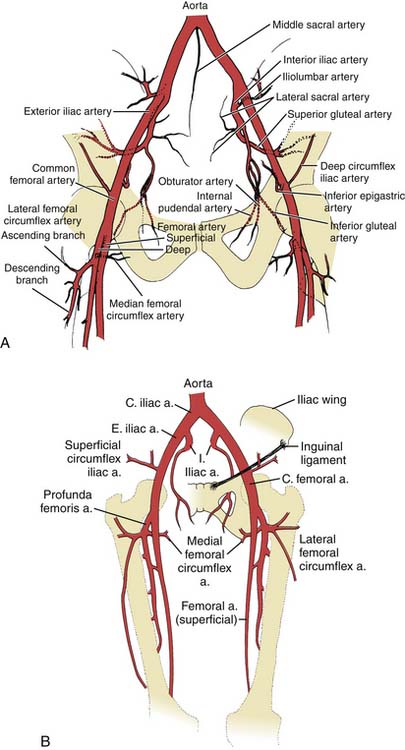
Familiarity with a variety of vascular access sites and techniques is one of the most important components of one’s basic skills in peripheral vascular intervention. Successful endovascular intervention requires the appropriate choice of vascular access. In most cases, access is obtained using a 21-gauge needle and 0.18-inch wire (4 F micropuncture set). The retrograde approach to the common femoral artery (CFA) is the most often used vascular access. Evaluation of the peripheral lower extremity disease requires identification of iliac bifurcation and common femoral artery patency (Fig. 5-8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree