Category
Description/prognosis
Findings
Doppler signals
Sensory loss
Motor loss
Arterial
Venous
I. Viable
Not immediately threatened
None
None
Audible
Audible
II. Threatened
(a) Marginally
Salvageable if promptly treated
Minimal (toes) or none
None
Inaudible
Audible
(b) Immediately
Salvageable with immediate revascularization
More than toes, associated with rest pain
Mild, moderate
Inaudible
Audible
III. Irreversible
Major tissue loss or permanent nerve damage inevitable
Profound, anesthetic
Profound, paralysis (rigor)
Inaudible
Inaudible
Imaging
The importance of a good clinical examination cannot be overstated. In a patient with imminent risk of limb loss, a well-performed clinical examination may provide enough diagnostic information to bring the patient directly to the operating room without wasting time on unnecessary imaging studies.
Duplex Ultrasound
Duplex ultrasound can accurately determine the level of obstruction and the status of other blood vessels in the limb. More importantly, in cases of aortic dissections extending into one extremity, duplex ultrasound can identify the true and false lumens.
Computed Tomography Angiography (CTA)
Computed tomography angiography (CTA) is widely available in most emergency departments, and the imaging quality is similar to intra-arterial angiography. As a noninvasive imaging modality, CTA has an advantage in the evaluation of aortoiliac occlusions, dissections, traumatic limb injuries, and patients with significant underlying occlusive disease.
Digital Subtraction Angiography (DSA)
Digital subtraction angiography (DSA) is the mainstay diagnostic study, especially when thrombolytic therapy is anticipated. An angiogram can show the level of occlusion, the patency of distal blood vessels. In some cases, the angiographic images suggest the etiology of ischemia. For example, embolic occlusions will have a sharp cutoff sign with no collateral vessels (Fig. 3.1), while thrombotic occlusions will show collateral blood vessels around the occluded artery (Fig. 3.2). For collaterals to develop, the affected artery must have been stenosis over a long period of time implying that the ischemic event represents acute thrombosis of an already diseased artery. Hybrid operating rooms allow for a seamless transition between diagnostic angiography, endovascular therapy, and surgical intervention.
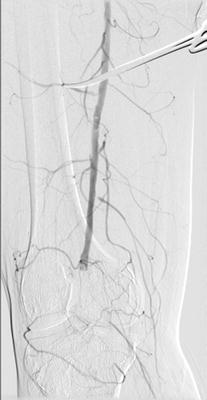

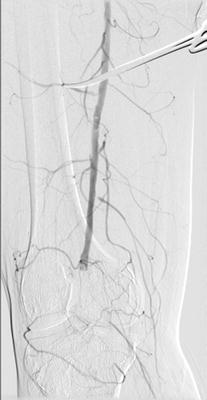
Fig. 3.1
Digital subtraction arteriogram showing embolic occlusion of the popliteal artery. Note the distinct cutoff of the popliteal and absence of collateral vessels

Fig. 3.2
Digital subtraction arteriogram showing arterial thrombosis with well-developed collaterals around the area of occlusion
Treatment Decision Making
Treatment decisions concerning an acutely threatened limb can be challenging for even the most experienced surgeons. Making the best treatment choice requires a basic understanding of the etiology, pathophysiology, and consequences of limb ischemia. Younger patients with acute limb ischemia are at risk for limb loss, whereas older patients have a high risk of mortality in addition to the threat of limb loss. Patients with acute myocardial infarction and poor cardiac output have substantially higher postoperative mortality, regardless of the type of operation performed [12, 13]. Therefore, performing a thorough history and physical examination and accurately placing the patient in the appropriate category of limb ischemia are crucial.
Anticoagulation should be initiated on all patients with acute limb ischemia. Blaisdell introduced the role of heparin in preventing proximal and distal propagation of thrombus in patients with acute limb ischemia [14]. Although heparin does not have thrombolytic properties, it stabilizes and prevents extension of the already formed thrombus while preserving the patency of the microcirculation. An initial heparin bolus of 80 units/kg should be followed by a continuous infusion of 18 units/kg/h. Most patients are dehydrated and benefit from large bore intravenous access and hydration. Contrast which is required for angiographic imaging may be harmful to kidney function, especially in dehydrated patients.
Patients with class I limb ischemia have viable limbs which allows more time to get investigational studies that will guide definitive treatment. Revascularization for this group of patients can be performed less emergently, and patients may benefit from anticoagulation in the interim period. In addition, high surgical risk patients occasionally are not revascularized if their residual perfusion is adequate and the addition of long-term anticoagulation is felt to prevent further ischemic events.
Patients with reversible ischemia (class II) require revascularization for limb salvage. The majority of patients with acute limb ischemia present as class II ischemia and benefit the most from revascularization efforts. Any sensory or motor deficit in this group of patients must be identified, as the presence of these deficits implies that the peripheral nerve cells are getting ischemic and will soon become anoxic. Nerve death is followed by muscle necrosis and limb loss. Patients with class IIa ischemia have marginally threatened limbs allowing the surgeon more time to decide on definitive treatment. All of these patients should be immediately anticoagulated and undergo an imaging study. Revascularization can involve endovascular or open surgical techniques, depending on the surgeon’s familiarity and comfort with the use of modern endovascular technology. The duration of symptoms can help guide treatment decisions. Patients who have less than 2 weeks duration of signs and symptoms benefit the most from endovascular treatment, while patients whose duration of symptoms is more than 2 weeks usually benefit more from open surgical procedures [15]. Intra-arterial thrombolytic therapy requires close clinical monitoring and interval angiography. If the patient cannot tolerate thrombolysis or develops worsening ischemia with motor loss, the treating surgeon must be prepared to perform an emergent open surgical revascularization to save the leg.
Patients with class IIb ischemia have acute critical ischemia and are at an extremely high risk for limb loss if emergent revascularization is not performed. Institutions with limited resources should consider transferring these patients to vascular centers of excellence which offer a full range of vascular and endovascular services. Evidence suggests that this strategy improves surgical outcomes in patients with acutely threatened limbs [3]. Historically, these patients had extremely high rates of limb loss. The advent of the embolectomy catheter by Fogarty in 1963 revolutionized the treatment of acutely threatened limbs [16]. Balloon catheter embolectomy became the gold standard surgical therapy for acute limb ischemia. Although low-dose intra-arterial thrombolytic treatment is effective for subcritical ischemia, the long treatment time required makes thrombolysis ill suited for threatened limbs requiring immediate reperfusion. Well-equipped endovascular centers can perform accelerated thrombolysis with high-dose, short-duration infusions [17] or pulse spray thrombolysis [18]. Use of these advanced techniques requires 24-h availability of angiography suites and a commitment to perform emergent open surgery if the limb status deteriorates during thrombolytic therapy. Patients with severe ischemia from a focal thrombus or embolus in a proximal vessel usually benefit more by proceeding directly to a definitive surgical thromboembolectomy.
Patients with class III acute limb ischemia have irreversible ischemia that cannot be treated with revascularization. In fact, revascularization attempts in this group of patients can be harmful by causing rhabdomyolysis and myoglobinuria. These patients are better served with limb amputation at the appropriate anatomic level.
Endovascular Therapy and Thrombolysis: General Principles
The use of thrombolytic therapy for acute limb ischemia has evolved over the last several decades with many reports in the literature describing its benefit. Systemic infusion of thrombolytic therapy has given way to catheter-directed thrombolysis (i.e., percutaneous placement of a catheter directly into the intra-arterial thrombus). Tissue plasminogen activator (TPA) has largely replaced streptokinase and urokinase and is infused in a variety of doses and infusion times. Although randomized trials have been performed, they failed to provide a clear-cut answer to the treatment dilemma of thrombolysis versus surgical revascularization. Meta-analyses have found similar mortality and amputation rates for both percutaneous thrombolysis and open surgery. Thrombolysis reduces the need for open major surgery at a cost of causing more bleeding and distal embolization [19, 20].
Patients who present with limb ischemia less than 14 days duration with intact motor and sensory function may benefit from intra-arterial catheter-directed thrombolysis followed by correction of the causative lesion. Treatment options for patients with an acutely occluded bypass graft include surgical graft thrombectomy, thrombolysis with correction of the causative lesion, or creation of a new bypass. Consideration needs to be given to the age of the graft, conduit availability, the duration and degree of ischemia, and the overall condition and comorbidities of the patient.
Absolute contraindications to thrombolysis are recent intracranial or retinal surgeries. The practitioner must be ready to abort thrombolysis in favor of open surgical revascularization if at any point thrombolysis is causing an unacceptable delay in revascularization. The decision to perform thrombolysis versus open surgical revascularization should be made by a surgeon familiar with both techniques in a center equipped to perform either procedure.
Femoral and Brachial Embolectomy Techniques
Femoral Artery Embolectomy
The majority of patients presenting with acute lower extremity ischemia have an embolism lodged at the common femoral artery bifurcation that can be surgically treated with a femoral embolectomy. All patients should receive full systemic heparinization while being prepared for emergent surgery. The operation can be performed under general anesthesia; however, local anesthesia with moderate sedation may be more appropriate for patients with significant pulmonary comorbidities. The sterile prep should extend from the umbilicus to the entire limb circumferentially down to the toes. A longitudinal or oblique incision can be made for femoral artery exposure. An oblique incision, while sometimes limiting exposure, is preferred by many surgeons for its superior healing especially in morbidly obese patients. Although oblique incisions can be associated with lymphatic issues such as lymphocele or lymphedema, these complications can be avoided by dissecting in a vertical plane once the superficial fascia has been opened.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


