Perioperative Care of the Patient Undergoing Lung Resection
The postoperative care of any patient who undergoes pulmonary resection starts long before the incision is made and comprises three main areas. The first is patient selection, the second is the actual operation itself, and the third is postoperative care. This chapter briefly reviews some of the specifics that go into these three areas. In addition, it discusses the incidence, prevention, and treatment of some of the most common postoperative problems that continue to vex thoracic surgeons around the world.
PATIENT SELECTION
Perhaps the best way to minimize postoperative complications is to operate only on young healthy patients. Unfortunately, thoracic surgeons, like most other surgeons, are now presented with older and sicker patients with increasing comorbidities. The median age of our society has increased and so has obesity and patients with chronic pain syndromes. We are increasingly challenged with larger tumors in older patients with smaller pulmonary reserve. As the bar for the upper age limit has been raised, the threshold for the acceptable FEV1% and DLCO % has fallen. Currently there are few, if any, absolute contraindications to pulmonary resection based on chronological age or pulmonary function.
MORBIDITY AND MORTALITY
During the perioperative period, many factors contribute to pulmonary compromise. Estimates of the overall surgical mortality for pulmonary resection range in large series from 2% to 4%. The estimated mortality increases with the size of the resection—from less than 1% for a wedge resection of the lung, to 2% to 3% for a lobectomy, and 6% to 8% for a pneumonectomy.
The morbidity associated with elective pulmonary resection is also high. Complications have been reported to occur in 36% to 75% of patients undergoing pneumonectomy and 41% to 50% of patients after lobectomy. Most complications are minor and include air leak, atrial fibrillation, and atelectasis. However, a significant number are major; these most commonly include pneumonia, aspiration, respiratory failure, myocardial infarction, bronchopleural fistula (BPF), and pulmonary embolus.
PREOPERATIVE ASSESSMENT AND OPTIMIZATION
Preoperative evaluation focuses on assessment of pulmonary function and its optimization, evaluation of cardiac status, and careful consideration of issues related to quality of life.
 LUNG FUNCTION
LUNG FUNCTION
Assessment of the patient’s risk for pulmonary resection starts preoperatively in the clinic. One important but difficult factor to quantify is the patient’s desire to undergo the work required to recuperate from a thoracic surgical procedure. The importance of walking and deep breathing after lung resection cannot be overstated. A study performed by the Lung Cancer Study Group suggested that the patient’s attitude toward his or her malignancy was the best indicator of long-term survival.1 A patient who appears to be unwilling to participate in his recovery should be allowed ample opportunity to explore reasonable alternative therapies, such as radiation. Moreover, if this attitude persists, it may be best not to operate at all.
A large number of studies have examined preoperative factors that predict postoperative risk to a patient. In a study of 476 patients operated on over 12 years, only 3 of 7 preoperative risk factors for morbidity and mortality were found to carry a significant association with mortality.1 These risks were age older than 60 years, pneumonectomy, and the presence of ventricular premature contractions on the preoperative electrocardiogram. All risk factors analyzed together accounted for only 12% of the risk of mortality. At the time of the initial visit, an attempt to establish the amount and character of sputum production, the presence or absence of an effective cough, and a patient’s ability to climb a flight of stairs of fixed height help provide an idea of a patient’s ability to undergo surgery. Patients with preoperative arterial hypercapnia are apt to have pulmonary hypertension and are poor candidates for pneumonectomy, but they may be able to tolerate a lobectomy. Pulmonary function tests, in particular the FEV1% and the DLCO %, in combination with lobar perfusion scans, allow prediction of the postoperative predicted or postresectional FEV1% (Fig. 105-1). A postresectional FEV1% less than 40% of predicted is a cause for concern. A study of the DLCO % in 165 patients who underwent lung resection identified it as the most important indicator of postoperative pulmonary complications or death.2 Another study focused on the maximal oxygen consumption (MVO2). An MVO2 of 20 mL/kg/min was associated with the fewest chance of complications, whereas an MVO2 less than 15 mL/kg/min was associated with a 75% postoperative morbidity rate.3
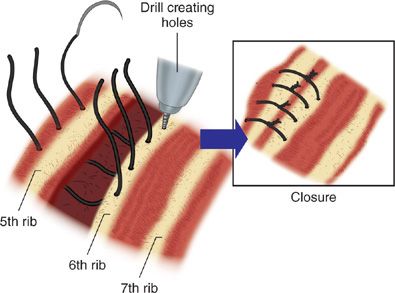
Figure 105-1 Drilling holes in the bottom rib, thus enabling sutures to be placed through it.
 CARDIAC STRESS TEST
CARDIAC STRESS TEST
Since many patients are smokers and elderly, we prefer to perform a preoperative stress test in most patients prior to thoracotomy. Previously undiscovered or unsuspected coronary artery disease should be determined, anatomically identified, and corrected prior to elective thoracotomy.
 QUALITY OF LIFE CONSIDERATIONS
QUALITY OF LIFE CONSIDERATIONS
Quality of life (QOL) is an important metric by which to assess all types of medical and surgical treatments. This is no different for patients who undergo pulmonary resection. In fact, QOL is becoming an increasingly important part of the preoperative conversation between patients and surgeons in planning out the procedure.4 For this reason smaller resections such as segmentectomy are becoming more common especially for tumors that are less than 2 cm in size. Similarly, pneumonectomy is less commonly performed. Recently we evaluated the long-term QOL in 110 patients who underwent a pneumonectomy and found that their overall physical scores were quite low but their mental well-being scores were high.5
 OPTIMIZATION OF PREOPERATIVE PULMONARY FUNCTION
OPTIMIZATION OF PREOPERATIVE PULMONARY FUNCTION
A variety of medical therapies are designed to improve pulmonary function. Many patients who are to undergo elective pulmonary resection are current smokers. Optimization of pulmonary function begins first and foremost with smoking cessation. Even a short period of abstinence from cigarettes can improve the effectiveness of mucociliary transport. Heavy smokers also maintain high levels of carboxyhemoglobin that interfere with oxygen transport and delivery to peripheral tissues. However, the optimal time after smoking cessation for elective thoracotomy is still unknown. In patients with evidence of reversible airway obstruction on pulmonary function tests, or symptoms suggestive of airflow obstruction, nebulized albuterol appears to be of benefit. Mucostasis, if present, may warrant the addition of mucolytics such as N-acetylcysteine. However, this medication may also lead to certain side effects, such as increased mucus production and bronchoconstriction. Similarly, although the condition of patients with reversible airflow obstruction generally improves with corticosteroids, these agents should be added cautiously because of their adverse effects on wound healing and the increased risk of wound infection. If steroids are necessary, the dosage in the postoperative period should be minimized. Patients who produce purulent sputum should be treated with oral antibiotics directed at the organism identified and surgery delayed until the infection is eradicated.
PERIOPERATIVE FACTORS REDUCING CARDIOPULMONARY FUNCTION
Despite the wide variety of pathologies and types of operative procedures performed by thoracic surgeons, the postoperative course is often quite predictable. We have published the techniques and specific steps that enable patients to be “fast-tracked” after both elective pulmonary resection and esophageal resection.6,7 These clinical pathways and/or computerized algorithms lead most importantly to safe results, high patient satisfaction, and only a 3- to 4-day length of stay after pulmonary resection. Early ambulation and aggressive pulmonary rehabilitation are cornerstones for successful fast-tracking. The physiological consequences of decreased activity and lack of changes in posture form a background for the pathophysiological processes caused by the underlying illness and the surgical procedure.
It is interesting that these changes might be less in patients with chronic pulmonary disease. Thus, in patients with chronic airflow obstruction, a decrease in FRC of only 3.5% accompanies a move from the upright to supine position and a decrease of only 1.9% accompanies the move from the supine to lateral decubitus position.8 Finally, although arterial oxygen saturation decreases significantly in supine normal subjects, it does not do so in patients with significant airflow obstruction.
The degree to which the described changes affect gas exchange has been only partly studied. In normal young males after 10 days of bed rest, PaO2 decreased by 9 mm Hg and the alveolar–arterial difference in Po2 by 10 mm Hg, without change in PaCO2. Such changes, which would probably not be important in normal young people, might take on greater significance in a patient with chronic obstructive pulmonary disease (COPD).
 BED REST AND CARDIAC FUNCTION
BED REST AND CARDIAC FUNCTION
Upon standing, approximately 500 mL of blood shifts from the upper to the lower body. When lying down, the central venous return increases, resulting in a decrease in heart rate, peripheral vasodilation, increased renal blood flow, and diuresis. Within an average of 24 hours the diuresis causes a 5% decrease in plasma volume, which continues to fall by 10% in 6 days and 20% in 14 days.
A wide variety of experimental subjects and protocols have been used to examine the cardiovascular effects of prolonged immobilization. Orthostatic intolerance is common after prolonged bed rest. This is attributable, at least in part, to the depletion in intravascular volume. This may be compounded by an increase in venous pooling in the lower extremities because of an increase in venous compliance after bed rest. Prolonged recumbency also blunts cardiac responsiveness to rapid changes in posture. Bed rest increases the resting heart rate by 4 to 15 beats per minute. After prolonged bed rest, the increase in heart rate during exercise is more pronounced. For example, normal volunteers experienced an increase in heart rate to approximately 129 beats per minute during submaximal exercise; after bed rest, the same exercise drove the heart rate to approximately 165 beats per minute.
 ALTERATIONS IN LUNG FUNCTION SECONDARY TO SURGERY
ALTERATIONS IN LUNG FUNCTION SECONDARY TO SURGERY
In addition to the physiological consequences of inactivity described in the preceding section, the thoracic surgery patient also experiences major alterations in chest wall compliance. The pain and discomfort of deep breathing also lead to an increase in the work of breathing that is independent of the amount of resected lung. Manipulation of the lung and re-expansion of the lung lead to pulmonary “bruising.” Microscopic or even macroscopic areas of atelectasis persist. Fluid or blood clots in the pleural cavity may compress the lung parenchyma. Inhalational anesthesia depresses mucociliary transport. Mechanical changes alter the work of breathing. Thoracotomy alone was found to decrease chest wall compliance to 47% of preoperative levels and to increase the work of breathing to 143% of preoperative levels.9 As a result, vital capacity and oxygen saturation fall significantly in the first few postoperative days. Pain, among other factors, leads to diminished cough. Cough pressures were found to decrease to 29% of preoperative levels after surgery and to increase only to 50% of preoperative levels by the seventh postoperative day.
ROUTINE POSTOPERATIVE CARE
Routine post-operative care focuses on decisions regarding timing of extubation, use of supplemental oxygen, judicious use of antibiotics, and fluid and electrolyte management. Additionally, radiographic evaluation and decisions regarding use and removal of chest tubes are important considerations.
 EXTUBATION AND POSTOPERATIVE SUPPLEMENTAL OXYGEN
EXTUBATION AND POSTOPERATIVE SUPPLEMENTAL OXYGEN
Almost every patient undergoing lung resection should be extubated in the operating room and brought to the recovery room breathing spontaneously. Reintubation in the immediate postoperative period is rare. If prolonged intubation is anticipated, however, the double-lumen endotracheal tube should be replaced by a single-lumen endotracheal tube of sufficient size to permit the introduction of an adult bronchoscope. For extubation, standard criteria are followed: vital capacity more than 10 mL/kg, respiratory rate less than 30 breaths per minute, and acceptable arterial blood gases.
Supplemental oxygen is supplied in the postoperative period if the patient’s arterial oxygen saturation, measured by pulse oximetry, is less than 90%, either at rest or during exercise. We prefer sending patients directly to the floor and have not used the intensive care unit after lobectomy for over a decade. Many centers have adopted a similar practice; however, patients must have 24-hour telemetry and pulse oximetry monitoring in these specialized units. Nurses need to have chest tube training. These types of floors allow the patient’s family to stay in close proximity at all times. This offers significant psychological support to most patients; if the family is attentive and intelligent, they also can act as an invaluable part of the patient’s care and add another level of patient protection.
 PAIN CONTROL
PAIN CONTROL
Adequate pain control in the postoperative state is critically important. The choice of surgical procedure and analgesic strategy to be employed are discussed below.
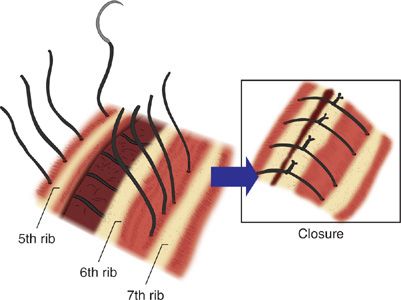
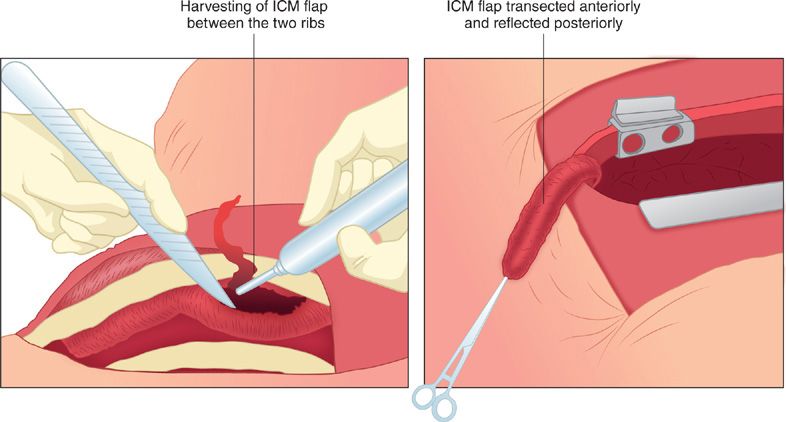
Impact of Surgical Techniques on Postoperative Pain
A thoracotomy is a painful procedure, in part related to trauma and/or compression of the intercostal nerve. We have evaluated ways to reduce the pain of thoracotomy using prospective randomized studies. One study showed that drilling holes in the bottom rib, thus enabling sutures to be placed through it rather than around the ribs, helps avoid entrapment of the lower intercostal nerve (Fig. 105-1) and this simple technique reduces the pain compared with the standard pericostal sutures (Fig. 105-2).10 Another study examined the use of an intercostal muscle flap.11 This flap is harvested prior to rib retraction (Fig. 105-3) so as to avoid retractor injury to the intercostal nerve, which runs in the muscle flap. Both of these studies showed reduction in postoperative pain in the hospital and a lessening of a decrease in the tidal volume immediately postoperatively. In addition, there was less pain at 3 months, both early and up to 12 weeks postoperatively. Simple techniques such as these, as well as video-assisted procedures that help prevent or limit the amount of pain are important.
Figure 105-2 Standard pericostal sutures.
Figure 105-3 Muscle flap harvested prior to rib retraction.
Postoperative pain is reduced through minimally invasive surgical approaches such as the use of video-assisted thoracoscopic surgery (VATS) and thoracic robotic surgery. Advantages of the robot in comparison to VATS include easier operations in the mediastinum, such as a thymectomy or a resection of an esophageal leiomyoma. Other potential advantages are improved lymph node resection and the dissection of enlarged or metastatic N1 lymph nodes off the pulmonary artery. However, there are significant limitations and concerns to the implementation of a robotic approach including the high cost, the lack of consistent platform availability, the lack of tactile feedback, the fact that several countries cannot afford the current robotic system, the need for the bedside assistant to fire the stapler on pulmonary vessels, and the lack of standardized credentials and training programs for the surgeons and technical assistants.
Analgesic Strategies
Postoperative pain that is not controlled early reduces the ability to breathe and cough and increases respiratory complications. Moreover, the best way to reduce late or chronic pain is to aggressively treat early pain. Most patients should receive a thoracic epidural prior to thoracotomy and/or a patient-controlled analgesic (PCA) intravenous device. Recently, some surgeons have tried subpleural catheter systems that infuse local anesthetics in the paravertebral area as well. The complications associated with epidural opiates are numerous and include pruritus, ileus, urinary retention, and respiratory depression. Epidural analgesia is most useful in the young patient with poor pulmonary function. We have avoided it in elderly patients, those who become somnolent, or those who have a rising carbon dioxide level on arterial blood gas. The use of nonsteroidal agents such as oral ketorolac in addition to narcotics is helpful as well and should be given immediately in the operating room and continued for a few days to help prevent pain. It should be avoided in those with marginal renal function. After postoperative day 2 or 3, the epidural should be removed and oral opioids should be added. Treating pain using a combination of different classes of agents is helpful.
 ANTIBIOTICS
ANTIBIOTICS
Wound infection following thoracotomy is rare. This may be due to the large amount of musculature contained in the chest wall. In addition, prophylactic antibiotics are often given in an attempt to reduce the incidence of wound infection. Currently, it is recommended that a broad-spectrum antibiotic, such as cefazolin, be administered within 1 hour of the skin incision. Subsequent antibiotic administration should be based on clinical factors such as fever, radiographic pulmonary infiltrates, leukocytosis, and sputum Gram stain and culture results. There is no need to provide antibiotic coverage simply because a chest tube is in place.
A study that examined the relationship between pulmonary flora and postoperative infections found that Haemophilus influenzae was the most common organism identified from sputum at the time of surgery and that the risk of pneumonia in culture-positive patients was 10-fold that of patients with culture-negative secretions.12 However, the cultured organisms were sensitive to the antibiotic that was administered, suggesting that the administration of antibiotics may be less important than careful pulmonary toilet in preventing postoperative pneumonia.
 FLUIDS, ELECTROLYTES, AND ORAL INTAKE
FLUIDS, ELECTROLYTES, AND ORAL INTAKE
A routine lung resection is not associated with large fluid losses intraoperatively or sequestration of volume in the third space postoperatively. Most patients should leave the operating room relatively euvolemic. Administration of intravenous fluids consisting of 5% dextrose and 0.45% normal saline at 50 to 75 mL/h until the patient begins to take oral fluids is usually adequate to maintain intravascular fluid volume. Oral intake should be resumed as soon as the patient is able to take fluids by mouth, but strict aspiration precautions cannot be overemphasized. Urine output should be maintained at 0.5 to 1 mL/kg of body weight an hour to preserve renal function. Oliguria, which is often overtreated by surgical residents, should be tolerated in patients who have undergone elective pulmonary resection. Some surgeons practice aggressive diuresis with the goal of reducing secretions. However, it is not clear that a lower volume of thick, tenacious secretions is preferable to a higher volume of thin secretions that are more readily cleared. Ideally, diuresis should be guided by measurements of intravascular volume. Measurements of central venous pressure correlate poorly with intravascular volume. Many surgeons are reluctant to insert Swan–Ganz catheters into patients after lung resection, particularly after pneumonectomy, because of the possibility of disruption of a pulmonary artery closure. Even if a Swan–Ganz balloon-tipped catheter has been safely introduced into a patient postoperatively, the data should be interpreted with caution because the inflated balloon may have occluded a significant portion of the remaining pulmonary vascular bed, thereby artificially increasing right ventricular afterload and decreasing cardiac output. In our practice the measurement of central venous pressure is rarely if ever used and a Swan is reserved for a patient in the intensive care unit that is hypotensive, oliguric, and hypoxic.
Blood transfusion is not necessary unless the patient’s hemodynamics and overall clinical scenario call for it. Some believe that a hematocrit less than 24% is an indication for transfusion, but we prefer to use the hemoglobin level, which is less affected by dilution. A decision should be made on each individual patient’s situation and a knee-jerk reaction to any specific level should be avoided. Transfusion of 250 mL of packed red blood cells increases the intravascular volume by 750 to 1000 mL, because of the movement of extravascular volume into the intravascular space due to plasma oncotic forces. The increase in intravascular volume may be more dangerous than low hemoglobin. Furthermore, the intraoperative administration of blood is probably immunosuppressive and may be associated with a decrease in frequency of 5-year disease-free intervals.
 ROUTINE CHEST X-RAYS
ROUTINE CHEST X-RAYS
We have studied the use of daily chest radiographs, which most surgeons perform to ensure the effective removal of air and fluid from the pleural space.13 These films, which are labor intensive, costly, and wake the patient in the early morning hours, are not needed if the patient does not have an air leak or other clinical problems. If the postoperative chest roentgenogram in the recovery room after surgery has no significant pathology and the patient is not hypoxic, a daily chest X-ray is not needed. If a patient develops subcutaneous emphysema and hypoxemia and there is a pneumothorax, then suction should be added.
 CHEST TUBES
CHEST TUBES
Chest tubes are commonly placed after thoracotomy to drain blood, serum, and air from the pleural space. The ideal number, type, or size of a chest tube to place after elective pulmonary resection is controversial. There are little data to suggest that one practice is better than another; however, recently several prospective randomized studies have shown that one chest tube works as well as two.14 After routine lobectomy we have changed our practice based on these studies and now only use one chest tube in patients who do not have a large untre atable air leak or a large fixed pleural space deficit after lobectomy. We use a 24-French soft catheter that is difficult to kink. The advantage of one tube is that it may cause less pain and morbidity, but this advantage is theoretical.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree