Fig. 20.1
The Memoir of Francisco Romero on the treatment of thoracic effusions as presented in 1815
20.3 Pericardial Effusions
The pericardium has many physiological functions which mainly prevent overdistension of the cardiac chambers and torsion of the heart by exerting a contact stress (Spodick 1991). However, congenital absence of the pericardium usually does not lead to specific clinical symptoms.
Under normal physiological conditions, only a minimal amount of pericardial fluid is present at the posterior side of the heart. Accumulation of fluid and/or air gives rise to specific conditions which are listed in Table 20.1. An example of air building up inside the pericardium, a so-called pneumopericardium, is provided in Fig. 20.2. A number of disorders may provoke pericardial effusions, and these are summarised in Table 20.2 (Hazelrigg and McGee 1999; Spodick 1991). When the volume of fluid increases in the pericardial space, depending on the amount and rate of accumulation, the pericardial reserve volume is exceeded and the pericardial pressure rises steeply which will ultimately result in cardiac tamponade. This occurs earlier when blood accumulates inside the pericardium and compresses the heart. Symptoms of a pericardial effusion include cough, shortness of breath, thoracic pain, malaise, peripheral oedema and symptoms related to the underlying disorder, e.g. cachexia in malignant pericardial effusions.

Table 20.1
Specific conditions in which air and fluid accumulate inside the pericardium
Pneumopericardium (tension) | Air (pneumotamponade) |
Hydropericardium | Serous fluid (transudate) |
Hydropneumopericardium | Air + serous fluid |
Haemopericardium | Blood, clots |
Pyopericardium | Purulent effusion |
Pyopneumopericardium | Purulent effusion + air |
Chylopericardium | Chyle |
Lymphopericardium | Lymphatic fluid |

Fig. 20.2
Postoperative pneumopericardium in a patient who underwent a left repeat thoracotomy for recurrent pulmonary metastases
Table 20.2
Disorders associated with pericardial effusions
Infectious | Viral, bacterial, mycotic, parasitic |
Traumatic | Penetrating, blunt |
Malignant | Primary |
Secondary (lung, breast, lymphoma) | |
Inflammatory | Connective tissue disorders |
Vasculitis | |
Metabolic | Renal failure |
Cholesterol pericarditis | |
Idiopathic/others | Cardiac surgery |
Intrapericardial pneumonectomy | |
Post-radiotherapy |
Chest X-ray usually reveals a clearly enlarged cardiac silhouette, typically with a water bottle configuration (Fig. 20.3). Electrocardiography may show reduced voltage, ST segment elevation and cardiac arrhythmias in cases with associated heart disease. Echocardiography readily provides the correct diagnosis and is able to differentiate between small, moderate and large effusions (Fig. 20.4). CT scan and magnetic resonance imaging may also be helpful to evaluate the pericardial thickness and cardiac function especially in patients with poor echogenic windows (Fig. 20.5). In some cases, the healing process will result in excessive thickening of the pericardium, associated fibrosis and constriction, which may finally give rise to a constrictive pericarditis characterised by a so-called Pantserherz (Fig. 20.5). This results in profound haemodynamic consequences by limiting normal filling of the cardiac cavities.

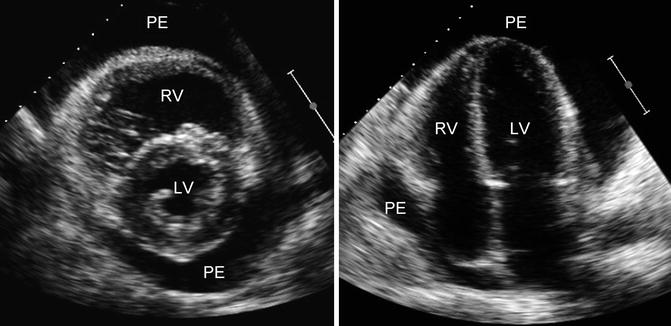
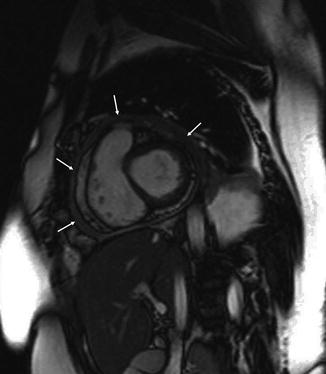

Fig. 20.3
A chest radiograph showing enlarged cardiac shadow due to a pericardial effusion post aortic valve replacement
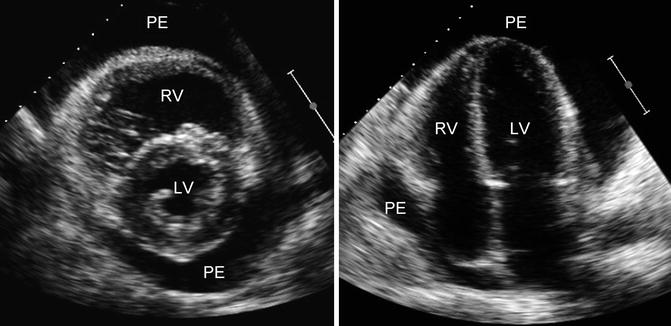
Fig. 20.4
Echocardiographic parasternal short axis (left panel) and apical four-chamber view (right panel) in a patient with large pericardial effusion (LV left ventricle, RV right ventricle, PE pericardial effusion)
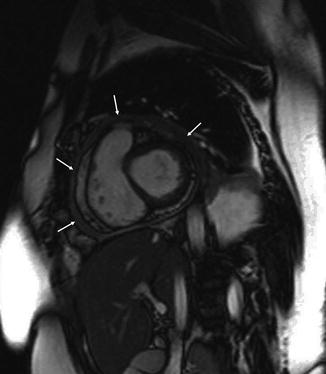
Fig. 20.5
Short-axis magnetic resonance image of the heart in a patient with constrictive pericarditis. The arrows indicate thickened pericardium (“Pantserherz”)
20.4 Surgical Approaches to the Pericardium
Several approaches to the pericardium exist, ranging from minimally invasive to extensive open procedures. These are listed in Table 20.3 together with their specific indication.
Table 20.3
Surgical approaches to the pericardium
Technique | Indication |
|---|---|
Anterior mediastinotomy with opening of the pericardium | Inspection, diagnosis pericardial + pulmonary disorders |
Videopericardioscopy | Inspection, evaluation intrapericardial lesions + biopsy |
Subxiphoid approach (surgical) | Drainage, pericardial biopsy, partial pericardial excision, pericardioperitoneal window |
Video-assisted thoracic surgery (VATS) | Diagnosis pleural, pulmonary, pericardial disorders; limited therapeutic interventions (pericardiopleural window)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|