Pericardial Disease
Wael A. Jaber • Parag R. Patel
QUESTIONS
1.A 62-year-old man is admitted with chronic obstructive pulmonary disease (COPD) and mild left ventricular (LV) dysfunction (ejection fraction [EF] 45%) as well as symptomatic, recurrent atrial fibrillation (heart rate [HR] 120s to 150s) despite antiarrhythmic drug therapy and direct current cardioversion in the past. After rate control with intravenous (IV) β-blockers, the HR improves and the patient feels better. Given his recurrent atrial fibrillation despite optimal medical therapy, the patient is referred for radiofrequency ablation of atrial fibrillation (pulmonary vein isolation) procedure. The procedure is performed on anticoagulation (international normalized ratio >2.0) and is deemed a success, with no inducible atrial fibrillation at the end of the case. A small atrial septal defect (ASD) was noted with intracardiac echocardiography at the end of the case, with no other remarkable findings. That evening in the post-anesthesia care-unit (PACU), the patient is noted to be hypotensive and tachycardic with increasing dyspnea. There is a concern for cardiac tamponade; however, the arterial line does not show a significant respiratory variation of the blood pressure (BP) waveform (pulsus paradoxus). An echocardiogram is performed, demonstrating a large circumferential effusion and the patient is referred for urgent pericardiocentesis. Which of the following explains why the patient did not develop a pulsus on the arterial line, despite a large, hemodynamically significant pericardial effusion?
a.Presence of an ASD
b.Administration of excess IV fluid during the ablation
c.LV dysfunction
d.COPD
2.A 38-year-old patient with no prior medical history presents to the emergency room with 4 days of chest discomfort. He denies any recent trauma, fever, or use of anticoagulants. The pain is positional and the patient reports mild upper respiratory infection (URI) symptoms in the preceding week. Laboratory work is notable for elevated white blood cell count (neutrophil predominance) as well as elevated erythrocyte sedimentation rate (ESR)/high-sensitivity C-reactive protein (hsCRP); his troponin and other laboratory work is otherwise negative/normal. Electrocardiogram (ECG) is consistent with pericarditis. There is a low suspicion for acute coronary syndrome, and acute pericarditis is diagnosed with small effusion on the echocardiogram; the pain improves with analgesics. Which of the following regimens is the most appropriate therapy for this patient to treat the acute episode and maintain remission?
a.Ibuprofen 600 TID for 2 weeks followed by taper and colchicine 0.5 mg BID for 3 months
b.Aspirin 325 daily and colchicine 0.5 mg BID for 2 weeks followed by taper
c.Ibuprofen 400 BID and colchicine 0.5 mg BID for 2 weeks followed by no taper
d.Prednisone 10 mg daily and ibuprofen 600 TID for 3 months followed by no taper
3.A 62-year-old man with cardiac risk factors of tobacco use, hypertension, and diabetes mellitus returns for follow-up after late-presenting mid-left anterior descending artery (LAD) ST-elevation myocardial infarction (MI). He had an occluded mid-LAD, which was successfully aspirated and stented with a single drug-eluting stent; no significant disease elsewhere is noted. The next day he reports progressive chest discomfort and mild fever and has developed a two-component pericardial friction rub on physical examination. His ECG is concerning for pericarditis (Dressler syndrome) and an echo is performed showing no interval change from discharge other than the presence of a small pericardial effusion. Which of the following regimens would be the most appropriate therapy in this patient?
a.Aspirin 650 TID for 2 weeks with taper to 81 mg daily + colchicine 0.5 mg BID for 3 months
b.Aspirin 325 daily for 2 weeks, then taper to 81 mg daily + ibuprofen 600 mg TID for 3 months
c.Ibuprofen 600 mg TID for 2 weeks with taper + colchicine 0.5 mg BID for 3 months
d.Indomethacin 50 mg TID for 3 months as well as aspirin 650 mg TID for 3 months with taper to 81 mg
4.A 45-year-old male patient with a history of acute pericarditis now returns for outpatient follow-up with increasing dyspnea and lower extremity edema. The patient was seen and started on high-dose aspirin and colchicine (no nonsteroidal anti-inflammatory drugs [NSAIDs] due to allergy) and has not been able to taper for the past 6 months due to persistent low-level symptoms. He has an elevated jugular venous pulse without inspiratory decline, 2+ pedal edema, and congested liver without ascites, as well as a soft pericardial knock. Laboratory values are notable for mild transaminitis as well as elevated ESR/hsCRP. ECG is unremarkable and echo shows a small persistent pericardial effusion with tubular-shaped LV with normal function, along with diastolic bounce and conical-shaped right ventricle (RV) as well as plethoric inferior vena cava and respirophasic transmitral and trans-tricuspid variation all consistent with constrictive pericarditis. Which of the following would be the next most appropriate step in management?
a.Initiate steroid therapy (0.25 to 0.5 mg/kg/day) along with colchicine, and initiate PO diuretic
b.Admit for IV diuresis and transition to PO diuretic regimen after cardiac catheterization for constriction evaluation
c.Repeat echo in 2 to 3 months aspirin and colchicine at current doses
d.Surgical evaluation for pericardiectomy/stripping
5.A 39-year-old patient with no prior medical visits presents with cardiac tamponade and undergoes urgent pericardiocentesis. He is from sub-Saharan Africa and has never been seen by a physician before—reports feeling progressively ill for the past month and brought to the hospital after syncopal episode today. Fluid analysis is performed and listed below:
Gram stain: no gram-positive/gram-negative bacteria noted
Peripheral cell count: normal (peripheral cell count <10 × 109 cells/L)
Pericardial fluid differential (lymphocyte/neutrophil): >1.0 (monocytes present as well)
Protein: elevated
hsCRP: markedly elevated
Lactate dehydrogenase (LDH): elevated (>2.0 times peripheral LDH level)
Adenosine deaminase (ADA): >40 U/L
Interferon gamma: >50 pg/mL
Glucose: low
Culture and cytology/acid fast staining: pending
The most likely etiology for the effusion would be
a.tuberculous pericarditis.
b.endemic malignancy (i.e., Epstein-Barr virus–associated Burkitt’s) with metastatic spread.
c.malarial (Plasmodium vivax).
d.unable to determine—require pericardial biopsy to confirm.
6.A 47-year-old man with constrictive pericarditis is undergoing an echocardiogram for follow-up. The sonographer asks you to explain the difference between the annulus reversus and annulus paradoxus phenomena. Which of the following statements is correct?
a.Annulus reversus refers to reversal of septal and lateral mitral tissue Doppler velocities (E′ septal > E′ lateral) and annulus paradoxus refers to inverse correlation of E/E’ and LV end-diastolic pressure.
b.Annulus reversus refers to reversal of septal and lateral mitral tissue Doppler velocities (A′ septal > A′ lateral) and annulus paradoxus refers to inverse correlation of E/E′ and LV end-diastolic pressure.
c.Annulus reversus refers to reversal of septal and lateral mitral tissue Doppler velocities (E′ septal < E′ lateral) and annulus paradoxus refers to positive correlation of E/E′ and LV end-diastolic pressure.
d.Annulus reversus refers to reversal of septal and lateral mitral tissue Doppler velocities (A′ septal < A′ lateral) and annulus paradoxus refers to a positive correlation of E/E′ and LV end-diastolic pressure.
7.A 51-year-old male patient is admitted to the hospital with anasarca and progressive dyspnea and functional limitation. He has a prior history of coronary artery bypass grafting and post-pericardiotomy syndrome with relapsing pericarditis that has likely advanced to constrictive physiology (despite slow taper steroid therapy), given his presenting symptoms and physical examination findings. During the admission he is aggressively diuresed with IV diuretics with improvement in his renal and liver function, as well as symptom improvement (edema and dyspnea). He is unable to go for a magnetic resonance imaging (MRI) for further assessment (prior metallic implant in his spine for scoliosis) and his echocardiogram images are technically difficult due to his distorted spine and prior cardiac surgery.
He is referred for dual transducer cardiac catheterization for hemodynamic evaluation of right- and left-sided pressures as part of his diagnostic workup. The catheterization laboratory team begins the procedure and calls you to discuss the case. They note a sinus rhythm at 90 bpm with occasional premature ventricular contraction and a central venous pressure of 4 mmHg and nonelevated end-diastolic pressures at the beginning of the study (due to recent diuresis); they are unable to elucidate diastolic equalization of pressures, significant “dip and plateau,” or respiratory discordance of the ventricular pressure waveforms.
A potential mechanism for the discordant catheterization findings would be
a.lack of preload due to overdiuresis.
b.borderline tachycardia and ectopy preventing accurate analysis.
c.presence of only mild constrictive physiology.
d.presence of restrictive cardiomyopathy and physiology.
8.A 32-year-old white man presented initially with low-grade fever, cough, and pleuritic chest pain. He was found on ECG to have diffuse ST-segment elevation. A transthoracic echocardiogram (TTE) revealed a large pericardial effusion, and serologies were positive for coxsackievirus B infection. He was diagnosed with acute viral pericarditis and treated with indomethacin. He returns 4 weeks later for follow-up and states that he no longer has any pain, but he notes some mild ankle swelling. His ECG is normal. A repeat TTE shows resolution of the effusion but new findings consistent with mild constriction. What is the next step in managing this patient?
a.Obtain cardiac MRI to better assess the pericardium.
b.Have a cardiothoracic surgical consultation for pericardiectomy.
c.Reassure the patient and observe him over the next 3 months for worsening of symptoms.
d.Start a course of steroids.
9.A 45-year-old woman with a history of treated carcinoma of the breast presents to the local emergency department with a few days of severe chest pain. In the emergency department, she appears ill and pale and in moderate discomfort. Her BP is 135/60 mmHg; her respiratory rate is 24 breaths per minute; her HR is 82 bpm; and her temperature is 100.8°F. The resident on call reads her chest X-ray (CXR) as unremarkable. Her ECG is shown in Figure 13.1. What is the most reasonable next step?
a.Give aspirin and nitroglycerin and prepare to administer thrombolytics.
b.Call the cardiac intervention team and rush the patient to the catheterization laboratory for emergency coronary intervention.
c.Give a nonsteroidal anti-inflammatory medication.
d.Discharge the patient and refer her for a gastroenterology follow-up as an outpatient.
10.A 59-year-old man with a history of coronary artery disease (CAD) and remote coronary bypass surgery presents with progressive dyspnea and vague chest pain. He had a stress echocardiogram for these symptoms that demonstrated normal LV function with no stress-induced wall motion abnormalities. However, he returned to the emergency department a few days later with recurrent symptoms. This time the house officer examining the patient notes 3+ pedal edema. The patient is admitted and started on diuretics. His blood tests are as follows:
White blood cell count = 11,000
Hemoglobin = 14.2
Platelets = 172,000
Albumin = 4.6
Urea = 11
Creatinine = 0.9
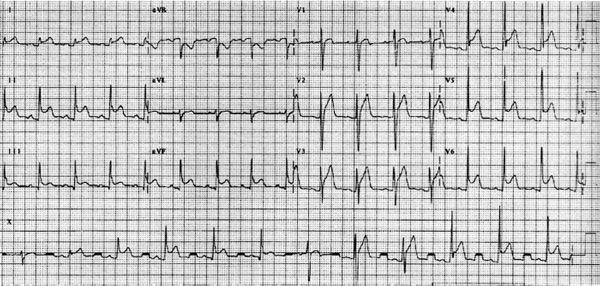
Figure 13.1 • (From Wagner GS, ed. Marriott’s Practical Electrocardiography, 9th ed. Baltimore, MD: Williams & Wilkins; 1994, with permission.)
Owing to the recurrent symptoms, his cardiologist decides to refer him for a right and left heart catheterization. The coronary grafts are all patent. The tracings from the study are shown in Figure 13.2. What is the most logical explanation for this patient’s symptoms?
a.Constrictive pericardial disease
b.Small-vessel CAD
c.Diastolic dysfunction related to his chronic CAD
d.Cardiac amyloid
e.Cardiac tamponade
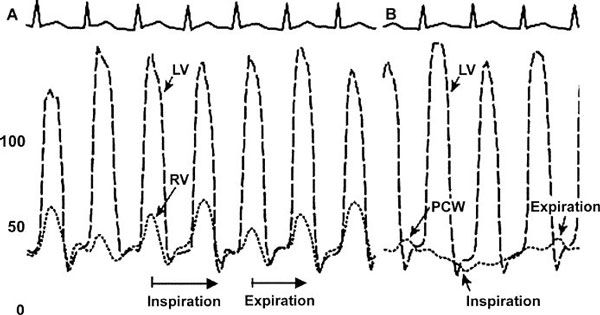
Figure 13.2 • PCW, pulmonary capillary wedge.
11.A 73-year-old man with no cardiac history presents with chronic lower extremities edema. His primary care physician attributed his symptoms to old age. He was treated with hydrochlorothiazide. Initially, he reported a good response to the therapy, but, over the past few months, his edema recurred, and doubling the diuretic dose did not alleviate his symptoms. On his initial examination, you notice distended neck veins and a quiet precordium. He has mild hepatomegaly and 4+ pedal edema. A TTE is suboptimal because of the patient’s inability to lie flat and obstructive lung disease. His blood work is as follows:
White blood cell count = 6,000
Hemoglobin = 12.7
Platelets = 225,000
Urea = 43
Creatinine = 2.4
Albumin = 3.6
A cardiac catheterization is performed. He has normal coronary arteries with mild impairment in LV systolic function. The tracings from the study are shown in Figure 13.3. What is your explanation of his symptoms?
a.You agree with his primary care physician. You tell the patient that he probably has peripheral venous insufficiency.
b.This patient has significant diastolic dysfunction, and his prognosis is guarded.
c.This patient’s symptoms are due to the LV systolic dysfunction and volume overload.
d.This patient should be referred for surgical evaluation for possible pericardial stripping.
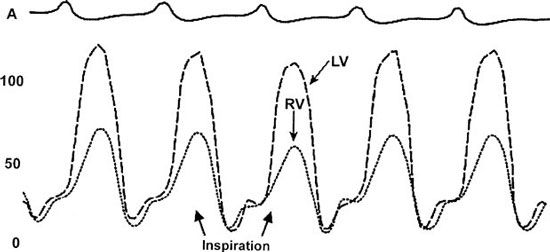
Figure 13.3 • Pressure tracings in the LV and RV.
12.A 56-year-old male smoker with a family history significant for CAD is presenting with dyspnea on exertion and nonexertional vague chest pain. His physical examination and his initial ECG are unremarkable. His CXR demonstrates an increased cardiac silhouette. There is also a small nodule seen in his right upper lobe. The radiologist is not certain about its significance. Given his risk factors and symptoms, he is referred for a perfusion stress test. The images from the stress test are shown in Figure 13.4. Which of the following does the patient clearly have?
a.He has coronary ischemia and should be referred for coronary angiography.
b.There is no evidence of pathology to justify his symptoms.
c.His symptoms are related to impairment of RV filling and pericardial disease.
d.He has mild ischemia and can be treated medically.
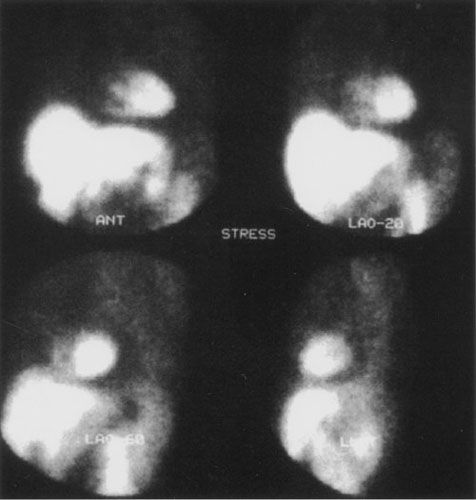
Figure 13.4 • (From Pohost GM, O’Rourke GA, Berman DS, et al., eds. Imaging in Cardiovascular Disease. Philadelphia, PA: Lippincott Williams & Wilkins; 2000, with permission.)
13.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


