Peribronchial Interstitial Thickening
Jud W. Gurney, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Acute and Chronic Bronchitis
Asthma
Aspiration
Cardiogenic Pulmonary Edema
Bronchiectasis
Sarcoidosis
Cystic Fibrosis
Less Common
Allergic Bronchopulmonary Aspergillosis
Langerhans Cell Histiocytosis
Chronic Hypersensitivity Pneumonitis
Cryptogenic Organizing Pneumonia
Lymphoma
Lymphangitic Carcinomatosis
Lymphocytic Interstitial Pneumonia
Rare but Important
Kaposi Sarcoma
Laryngeal Papillomatosis
Amyloidosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Normally 23 generations of airways from trachea to respiratory bronchiole
CT can visualize to 8 generation branches
Airways parallel course of arteries, both enclosed in connective tissue sheath known as peribronchovascular or axial interstitium
Components include airway and arterial wall and central lymphatics
Normally bronchi slightly smaller than artery (normal bronchoarterial ratio [B/A] = 0.65-0.70)
B/A > 1 seen in elderly (> 65 years old) or those living at high altitude (due to mild hypoxia that dilates bronchi and causes vasoconstriction)
B/A > 1.5 indicative of bronchiectasis
Helpful Clues for Common Diagnoses
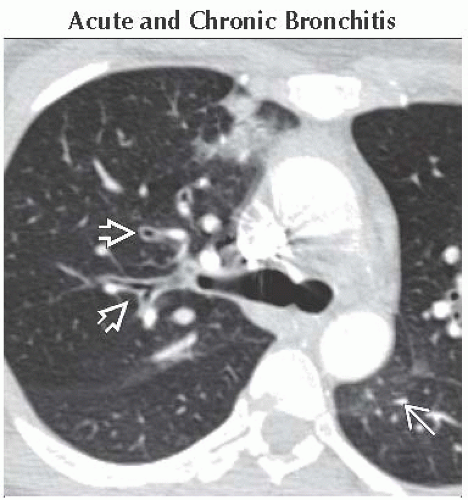
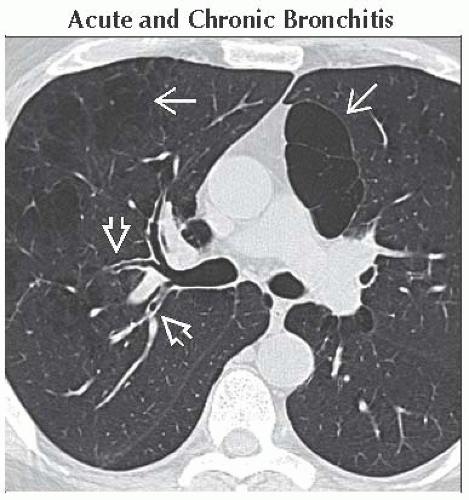
Acute and Chronic Bronchitis
Acute bronchitis usually secondary to viral upper respiratory infection; chronic bronchitis due to inhaled irritants (cigarette smoke and air pollution)
CT insensitive, nonspecific findings of smooth bronchial wall thickening, narrowed lumen, mucus-filled airway
Asthma
Reactive airways disease
Heterogeneous distribution in lung
Affects mainly small and medium-sized bronchi
Degree of bronchial wall thickening correlates with severity of airflow obstruction
Aspiration
Recurrent aspiration typically in elderly with neurologic disorders, dementia, or swallowing disorder
Gravity-dependent opacities
Consolidation and interstitial fibrosis centered on airways
Cardiogenic Pulmonary Edema
Smooth bronchovascular bundle thickening due to peribronchovascular edema
Usually seen with associated findings: Septal thickening, cardiomegaly, pleural effusions
Bronchiectasis
Integrity of bronchial wall dependent on normal immune system, normal structural integrity of airways (normal cartilage), and normal ciliary function
Bronchiectasis most commonly involves medium-sized bronchi of 4th-9th generations
Bronchi diameter larger than adjacent pulmonary artery: Cylindrical to saccular morphology
Focal or diffuse; when confined to 1 lobe, usually postinfectious or secondary to aspiration
Bronchial wall thickening may be absent even with dilatation
Sarcoidosis
Perilymphatic nodules (granulomas) along axial interstitium
Often associated with septal and subpleural nodules
Cystic Fibrosis
Bronchial wall thickening earliest finding, precedes development of bronchiectasis
Leads to diffuse bronchiectasis, usually more severe in upper lobes
Helpful Clues for Less Common Diagnoses
Allergic Bronchopulmonary Aspergillosis
Hypersensitivity reaction to Aspergillus fumigatus in asthmatics or cystic fibrosis
Central bronchiectasis, usually more severe in upper lobes
Langerhans Cell Histiocytosis
Strongly associated with smoking
Bronchocentric nodules evolving into cysts in upper and mid lung zones
Chronic Hypersensitivity Pneumonitis
Chronic granulomatous lung disease caused by inhalation of organic or chemical antigens
Chronic disease leads to fibrosis, usually centered on airways
Cryptogenic Organizing Pneumonia
Clinicopathological entity characterized by polypoid plugs of granulation tissue within airspaces
Most common pattern is multiple alveolar opacities (90%) centered on airways
Air-bronchograms common, often dilated
Other patterns: Multiple pulmonary nodules (may have air-bronchograms), solitary mass, perilobular pattern, reverse halo sign
Lymphoma
May be either non-Hodgkin or Hodgkin
Multifocal masses centered on airways with air-bronchograms
Masses are usually nonobstructive
Lymphangitic Carcinomatosis
Typically adenocarcinomas
Nodular or beaded thickening of bronchovascular bundles
Frequency of involvement: Axial (75%) > axial + peripheral (20%) > peripheral (5%)
Lymphocytic Interstitial Pneumonia
Spectrum of lymphoproliferative disorder
Ground-glass opacities, centrilobular nodules, and thin-walled cysts
Findings centered on lymphatic pathways: Peribronchovascular, septa, and pleura
Helpful Clues for Rare Diagnoses
Kaposi Sarcoma
AIDS-related neoplasm with propensity to involve skin, lymph nodes, GI tract, and lungs
Nodular perihilar thickening of bronchovascular bundles
Laryngeal Papillomatosis
Due to human papilloma virus, < 1% seed lung
Multiple solid or cavitated nodules centered on airways
Amyloidosis
Tracheobronchial most common form
Focal or diffuse thickening of airway wall with intraluminal nodules and submucosal foci of calcification
Image Gallery
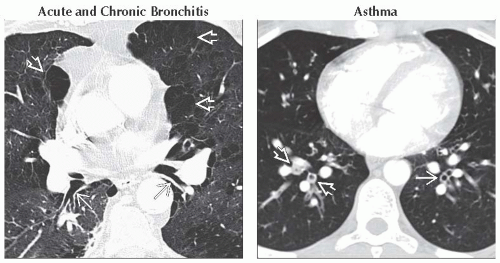 (Left) Axial NECT shows smooth thickening of the walls of the central bronchi
 from chronic bronchitis. Note the areas of emphysema from chronic bronchitis. Note the areas of emphysema  . (Right) Axial CECT shows diffuse bronchial wall thickening . (Right) Axial CECT shows diffuse bronchial wall thickening  and mucus plugging and mucus plugging  of subsegmental airways. Note that the distal lung is normal. Patient had acute asthma and had a study to rule out pulmonary embolus. of subsegmental airways. Note that the distal lung is normal. Patient had acute asthma and had a study to rule out pulmonary embolus.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|