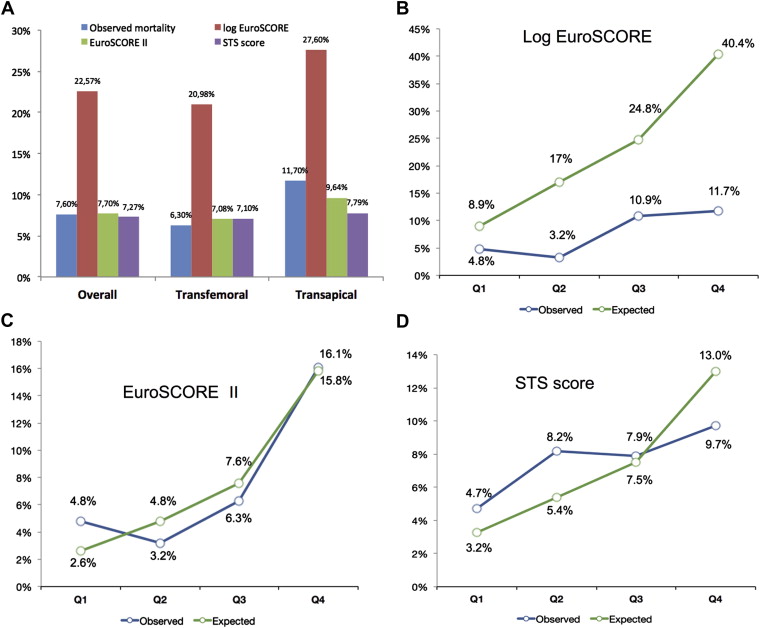
The original European System for Cardiac Operative Risk Evaluation (EuroSCORE) has been recently updated as EuroSCORE II to optimize its efficacy in cardiac surgery, but its performance has been poorly evaluated for predicting 30-day mortality in patients who undergo transcatheter aortic valve replacement (TAVR). Consecutive patients (n = 250) treated with TAVR were included in this analysis. Transapical access was used in 60 patients, while 190 procedures were performed using a transfemoral approach. Calibration (risk-adjusted mortality ratio) and discrimination (C-statistic and U-statistic) were calculated for the logistic EuroSCORE, EuroSCORE II, and Society of Thoracic Surgeons (STS) scores for predicting 30-day mortality. Observed mortality was 7.6% in the overall population (6.3% and 11.7% for the transfemoral and transapical cohorts, respectively). Predicted mortality was 22.6 ± 12.8% by logistic EuroSCORE, 7.7 ± 5.8% by EuroSCORE II, and 7.3 ± 4.1% by STS score. The risk-adjusted mortality ratio was 0.34 (95% confidence interval [CI] 0.10 to 0.58) for logistic EuroSCORE, 0.99 (95% CI 0.29 to 1.69) for EuroSCORE II, and 1.05 (95% CI 0.30 to 1.79) for STS score. Moderate discrimination was observed with EuroSCORE II (C-index 0.66, 95% CI 0.52 to 0.79, p = 0.02) compared to the logistic EuroSCORE (C-index 0.63, 95% CI 0.51 to 0.76, p = 0.06) and STS (C-index 0.58, 95% CI 0.43 to 0.73, p = 0.23) score, without a significant difference among the 3 risk scores. Discrimination was slightly better in the transfemoral cohort compared to the transapical cohort with the 3 risk scores. In conclusion, EuroSCORE II and the STS score are better calibrated than the logistic EuroSCORE but have moderate discrimination for predicting 30-day mortality after TAVR.
Surgical risk scores, such as the logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) and Society of Thoracic Surgeons (STS) predicted risk for mortality score, are commonly used to identify high-risk patients for surgical aortic valve replacement. A logistic EuroSCORE ≥20% and/or an STS score ≥10% are used to screen high-risk patients for transcatheter aortic valve replacement (TAVR). These 2 risk scores have also been evaluated for predicting mortality after TAVR. An updated version of the original logistic EuroSCORE model, EuroSCORE II, was recently validated in a contemporary cardiac surgical population. EuroSCORE II was better calibrated than the original logistic model, which overpredicted mortality. Moreover, very good discrimination was observed. The aim of this study was to assess the performance of EuroSCORE II for predicting 30-day mortality in patients who undergo TAVR, compared to the logistic EuroSCORE and the STS score.
Methods
From May 2006 to October 2011, 250 consecutive patients underwent TAVR at our center using the balloon-expandable Edwards SAPIEN and SAPIEN XT prostheses (Edwards Lifesciences, Irvine, California). All patients were included in a prospective, single-center registry. The patients were considered candidates for TAVR when the logistic EuroSCORE was ≥20%, in case of frailty (by agreement between cardiologists and cardiac surgeons), or in case of co-morbidities contraindicating surgical aortic valve replacement (porcelain aorta, chest irradiation, or deformation). All patients provided signed informed consent for subsequent data collection and analysis for research purposes.
The logistic EuroSCORE was prospectively calculated using an on-line calculator ( http://www.euroscore.org ) to estimate baseline surgical operative risk. In each patient, the STS score and the new EuroSCORE II were retrospectively calculated using web-based systems ( http://209.220.160.181/STSWebRiskCalc261/de.aspx and http://www.euroscore.org , respectively).
Table 1 lists the variables included in each risk model and highlights the differences among the algorithms. The logistic EuroSCORE is based on 12 covariates derived from 14,799 patients who underwent all types of cardiac operations (mostly coronary bypass) in 8 European countries in 1995. The STS score is based on 24 covariates derived from 67,292 patients in the United States over a relatively more contemporary period from 2002 to 2006. The EuroSCORE II has been recently established from 22,381 consecutive patients who underwent major cardiac surgery in 154 hospitals in 43 European countries over a 12-week period (May to July 2010).
| Variable | EuroSCORE | EuroSCORE II | STS Score |
|---|---|---|---|
| Age | X | X | X |
| Gender | X | X | X |
| Height | X | ||
| Weight | X | ||
| Body mass index | X | ||
| Diabetes mellitus | X | X | |
| Chronic lung/pulmonary disease | X | X | X |
| Mild/moderate/severe | X | ||
| Extracardiac arteriopathy | X | X | |
| Peripheral vascular disease | X | ||
| Neurologic dysfunction | X | ||
| Cerebrovascular accident | X | ||
| Poor mobility | X | ||
| Previous cardiac surgery | X | X | X |
| Number of previous operations | X | ||
| Previous coronary bypass | X | ||
| Previous valve surgery | X | ||
| Renal failure/impairment | X | X | X |
| Dialysis-dependent renal failure | X | X | |
| Serum creatinine/clearance | X | X | |
| Hypertension | X | ||
| Active endocarditis | X | X | X |
| Immunosuppressive therapy | X | ||
| Arrhythmia | X | ||
| Recent myocardial infarction | X | X | X |
| Timing | X | ||
| Cardiogenic shock | X | ||
| Inotropic agents | X | ||
| Intra-aortic balloon pump | X | ||
| New York Heart Association classification | X | X | |
| Unstable angina/Canadian Cardiovascular Society class IV angina | X | X | X |
| Critical preoperative state | X | X | |
| Left ventricular ejection function | X | X | X |
| Number of diseased coronary vessels | X | ||
| Left main coronary artery disease | X | ||
| Pulmonary hypertension (>60 mm Hg) | X | ||
| Moderate (31–55 mm Hg), severe (>55 mm Hg) | X | ||
| Procedure status/urgency | X | X | X |
| Weight of intervention | X | X | X |
| Single noncoronary bypass/2 or 3 procedures | X | X |
All the procedures were performed using the balloon-expandable Edwards SAPIEN valve from May 2006 to October 2009 and the SAPIEN XT prosthesis thereafter. The devices and procedures have been described previously.
Parameters were obtained at baseline, discharge, and 1 month, and the data were entered in our institutional prospective database. For patients from other institutions, outcomes at 30 days were obtained by telephone interview of the referring physicians and medical reports.
The primary end point was all-cause death at 30 days. Device success was defined according to the Valve Academic Research Consortium.
Qualitative variables are expressed as percentage and quantitative variables as mean ± SD or as median (interquartile range). The performance of the logistic EuroSCORE, EuroSCORE II, and STS score was evaluated in terms of their calibration and discrimination. Quartile distributions of observed and expected mortality for the 3 risk scores were also presented. Model calibration (the degree to which observed outcomes are similar to the expected outcomes from the model across patients) was examined by comparing average observed and predicted mortality. We first examined the Hosmer-Lemeshow test for goodness of fit within each of 10 equally sized subgroups in increasing order of patient risk. Hosmer-Lemeshow p values >0.05 indicate a well-calibrated model for the study population. Model calibration was also evaluated using the risk-adjusted mortality ratio (RAMR). An observed/expected ratio >1.0 indicates that the model underpredicts mortality, while an observed/expected ratio <1.0 indicates that the model overpredicts mortality. To gauge the statistical significance of the RAMR, we calculated the 95% confidence interval (CI) for the RAMR. If the 95% CI excluded the value 1.0, the RAMR was considered statistically significant, and the model was inadequately calibrated. In contrast, if the 95% CI included the value 1.0, the RAMR was not considered statistically significant, and the model was therefore well calibrated. Discriminatory power was assessed using the C-index (area under the receiver-operating characteristic curve [AUC]) and its 95% CI. A C-index of 0.5 indicates no predictive ability, whereas a C-index of 1.0 represents perfect discrimination. U-statistics were used to investigate differences in C-statistics across different scores. All data were analyzed using SPSS version 17.0 (IBM, Armonk, New York).
Results
During the study period, 250 patients underwent TAVR at our center. Transapical (TA) access was used in 60 patients (24%), while 190 procedures (76%) were performed using a transfemoral (TF) approach. Baseline characteristics of the study population are listed in Table 2 . Co-morbidities were more frequent in the TA cohort. Device success was 90.8%, without a significant difference between the TF and TA cohorts (92.1% vs 86.7%, p = 0.204). Thirty-day follow-up for the primary end point was 100%. There were 19 deaths at 30 days in the overall population (7.6%), 12 (6.3%) and 7 (11.7%) in the TF and TA cohorts, respectively. Causes of death are listed in Table 3 .
| Variable | Overall (n = 250) | TF (n = 190) | TA (n = 60) | p Value |
|---|---|---|---|---|
| Age (yrs) | 83 ± 7 | 84 ± 6 | 81 ± 7 | 0.002 |
| Men | 115 (46.0%) | 79 (41.6%) | 36 (60.0%) | 0.017 |
| Hypertension | 181 (72.4%) | 134 (70.5) | 47 (78.3%) | 0.32 |
| Diabetes mellitus | 64 (25.6%) | 50 (26.3%) | 14 (23.3%) | 0.74 |
| Previous myocardial infarction | 64 (25.6%) | 42 (22.1%) | 22 (36.7%) | 0.03 |
| Previous percutaneous coronary intervention | 70 (28.0%) | 47 (24.7%) | 23 (38.3%) | 0.05 |
| Previous coronary bypass | 49 (19.6%) | 28 (14.7%) | 21 (35.0%) | 0.001 |
| Atrial fibrillation | 96 (38.6%) | 79 (41.6%) | 17 (28.3%) | 0.07 |
| Pacemaker | 28 (11.2%) | 17 (8.9%) | 11 (18.3%) | 0.06 |
| Previous balloon aortic valvuloplasty | 103 (41.2%) | 77 (40.5%) | 26 (43.3%) | 0.76 |
| Peripheral artery disease | 55 (22.0%) | 21 (11.1%) | 34 (56.7%) | <0.001 |
| Porcelain aorta | 20 (8.0%) | 8 (4.2%) | 12 (20.0%) | <0.001 |
| Previous stroke | 14 (5.6%) | 10 (5.3%) | 4 (6.7%) | 0.75 |
| Creatinine (μmol/L) | 116 ± 56 | 113 ± 51 | 125 ± 69 | 0.23 |
| Chronic obstructive pulmonary disease | 74 (29.6%) | 57 (30.0%) | 17 (28.3%) | 0.87 |
| Chest irradiation | 24 (9.6%) | 20 (10.5%) | 4 (6.7%) | 0.46 |
| Neoplasia | 57 (22.8%) | 43 (22.6%) | 14 (23.3%) | 1.00 |
| New York Heart Association functional class III or IV | 188 (75.2%) | 145 (76.3%) | 43 (71.7%) | 0.50 |
| Mean aortic gradient (mm Hg) | 45 ± 17 | 46 ± 17 | 41 ± 14 | 0.06 |
| Aortic valve area (cm 2 ) | 0.65 ± 0.17 | 0.64 ± 0.17 | 0.68 ± 0.18 | 0.19 |
| Pulmonary artery systolic pressure (mm Hg) | 44.4 ± 14.0 | 43.7 ± 13.7 | 46.2 ± 15.1 | 0.31 |
| Left ventricular ejection fraction (%) | 55 ± 16 | 55 ± 17 | 56 ± 13 | 0.64 |
| Left ventricular ejection fraction <30% | 26 (10.4) | 24 (12.6) | 2 (3.3) | 0.05 |
| Age (yrs) | Interval from TAVR to Death (days) | Cause of Death | Logistic EuroSCORE (%) | STS Score (%) | Euro SCORE II (%) |
|---|---|---|---|---|---|
| TF | |||||
| 79 | 3 | Myocardial infarction | 24.4 | 7.5 | 9.1 |
| 79 | 1 | Sudden cardiac death | 23.3 | 5.7 | 9.0 |
| 82 | 0 | Aortic dissection | 21.2 | 7.1 | 19.6 |
| 85 | 1 | Sudden cardiac death | 31.7 | 4.6 | 4.2 |
| 87 | 5 | Sepsis | 25.6 | 17.7 | 24.1 |
| 91 | 27 | Sepsis | 26.3 | 6.0 | 14.5 |
| 80 | 9 | Annulus rupture | 22.7 | 14.2 | 6.5 |
| 88 | 0 | Ventricular fibrillation | 61.5 | 8.1 | 14.9 |
| 85 | 11 | Myocardial infarction | 38.9 | 19.1 | 20.3 |
| 80 | 5 | Acute respiratory failure | 24.7 | 8.3 | 16.2 |
| 87 | 6 | Acute respiratory failure | 20.4 | 21.0 | 10.9 |
| 85 | 0 | Annular rupture | 18.4 | 10.4 | 4.4 |
| TA | |||||
| 80 | 0 | Valve migration | 34.6 | 4.9 | 10.3 |
| 74 | 19 | Acute respiratory failure | 22.4 | 5.5 | 5.6 |
| 80 | 3 | Ventricular fibrillation | 42.5 | 24.7 | 6.8 |
| 91 | 5 | Heart failure | 10.7 | 2.7 | 2.2 |
| 90 | 17 | Sepsis | 37.8 | 19.8 | 12.3 |
| 89 | 0 | Valve migration | 31.2 | 4.7 | 11.2 |
| 87 | 6 | Heart failure | 9.5 | 2.4 | 3.0 |
Predicted mortalities in the overall population as well as in the TF and TA cohorts are shown in the Figure 1 . Calibration of the logistic EuroSCORE, EuroSCORE II, and STS score was evaluated using the Hosmer-Lemeshow goodness-of-fit test and the RAMR tests. The results are listed in Table 4 . The Hosmer-Lemeshow test indicated acceptable calibration for the 3 risk scores in the overall population as well as in the TF and TA cohorts (p values >0.05 for all evaluations), although the EuroSCORE overestimated mortality. The RAMR indicated that EuroSCORE II and the STS score, but not the logistic EuroSCORE, were adequately and significantly calibrated in the overall population, because the observed/expected ratios were close to 1.0 and the 95% CI included the value 1.0. Interestingly, these scores slightly overestimated mortality in the TF cohort and underestimated mortality in the TA cohort.