A 52-year old man was admitted with out-of-hospital cardiac arrest, and he was resuscitated after 100 minutes. The initial hemodynamic condition was critical due to cardiogenic shock (left ventricular ejection fraction 10 % and mean arterial pressure 60 mmHg on inotropics). Acute coronary angiography did not reveal any new lesions. Due to persistent hemodynamic instability, mechanical support with Impella LP 5.0 was decided. The surgical procedure guided by fluoroscopy and transesophageal echocardiography was uncomplicated. The hemodynamic improved subsequently and after 17 days of intensive care, and additional 30 days of hospitalization, the patient was ready for discharge. Routine echocardiography prior to discharge revealed severe mitral regurgitation due to perforation of anterior mitral leaflet, a finding not observed in the previous echocardiograms. The patient was discharged to close follow up of the severe mitral regurgitation and future surgical intervention is likely. Therefore, close monitoring of mitral valve is necessary and explanation may be required if valve dysfunction is observed, as repositioning of the Impella system is not possible.
The Impella is an axial rotary pump used for cardiogenic shock as temporary support for recovery or bridge to heart transplantation. It has an inlet area in the left ventricle and the outlet area in the ascending aorta cranial to the aortic valve. Three sizes exist: 2.5 L/min, 3.5 L/min and 5.0 L/min. The 2 smaller sizes are implanted with transfemoral access. Impella LP 5.0 (21 French) is implanted surgically through the right subclavian artery. The volume output of the Impella 5.0 is higher and allows a longer period of mechanical support.
Case report
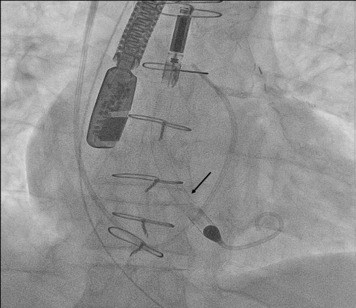
A 52-year-old man was admitted with out-of-hospital cardiac arrest. The initial rhythm was ventricular fibrillation. He had a history of stable coronary heart disease, chronic heart failure (ejection fraction 40%), and peripheral artery disease. Return of spontaneous circulation occurred after 100 minutes. Owing to an unstable hemodynamic condition, it was attempted to provide cardiopulmonary support with transfemoral access; however, this approach was abandoned because of heavy calcified deposits in the femoral artery. The coronary angiogram did not reveal any acute lesions. The mean arterial pressure was 60 mm Hg on medium doses of (0.3 and 0.05 μg/kg/min, respectively) norepinephrine and epinephrine. Echocardiography showed a left ventricular ejection fraction of 10% with no sign of mitral regurgitation. The patient deteriorated hemodynamically (lactate 19 mmol/L) despite increasing doses of norepinephrine 0.5 and epinephrine 0.14 μg/kg/min, respectively. The Impella 5.0 was chosen because of the subclavian access. The procedure was conducted surgically guided by fluoroscopy and transesophageal echocardiography ( Figure 1 ). There were no procedural complications. The Impella implantation resulted in rapid improvement of the hemodynamic condition ( Table 1 ). Initial echocardiographic control of the Impella showed the system was in close proximity to the anterior mitral leaflet, but there was no sign of regurgitation ( Figure 2 ). After 11 days, the overall condition stabilized and the Impella system explanted. The patient returned to the cardiac ward after 17 days of intensive care. There were no neurologic or cognitive deficits and renal function recovered. Routine echocardiography before discharge (after 47 days of hospitalization) revealed an ejection fraction of 25%, left ventricular dilatation (70 mm diastolic diameter), and unexpectedly severe mitral regurgitation. Transesophageal echocardiography confirmed the presence of severe mitral regurgitation because of development of aneurysm and perforation of the anterior mitral leaflet ( Figure 3 ). There were no signs of infection. The patient was discharged to close follow-up at our outpatient clinic. The severe mitral regurgitation persists and is likely to require future surgical correction when the patient’s general condition has improved.