34 Percutaneous Retrieval of Foreign Bodies in the Cardiovascular System
 Introduction
Introduction
As the use of implantable transient or permanent central venous catheters and probes increases, the number of catheter or probe fragments that accidently remain in the vascular system also increases. While historically the removal of foreign bodies was the domain of cardiac and vascular surgery, their extraction by interventional means continues to increase in significance.
In most of the cases referred to our center for foreign body extraction, patients have a dislocated and embolized port catheter, central venous catheter, or pacemaker lead. On rare occasions there are fragments of arterial catheters. As a result of modern stent technology the recovery of embolized, nonexpanded stents is a thing of the past and will not be discussed here.
The severed catheters are mainly found in the region of the superior vena cava and the right atrium, very rarely in the right ventricle or the pulmonary artery. The catheter fragments generally float in the area of the tricuspid valve and are highly mobile. Catheter fragments or pacemaker leads in the right atrium or ventricle are often heavily coiled.
 Indication
Indication
The need for extraction is determined by the risk of embolization into the pulmonary artery and the triggering of arrhythmias when located in the right atrium or ventricle, and especially by the danger of secondary bacterial colonization and the risk of endocarditis from
 Dislocated port catheter or central venous catheter
Dislocated port catheter or central venous catheter
 Dislocated pacemaker leads
Dislocated pacemaker leads
 Dislocated vena cava filter
Dislocated vena cava filter
 Dislocated coils and other implants
Dislocated coils and other implants
 Instruments
Instruments
 10F to 12F sheath
10F to 12F sheath
 6F to 7F guidewire (multipurpose)
6F to 7F guidewire (multipurpose)
 6F to 7F pigtail catheter
6F to 7F pigtail catheter
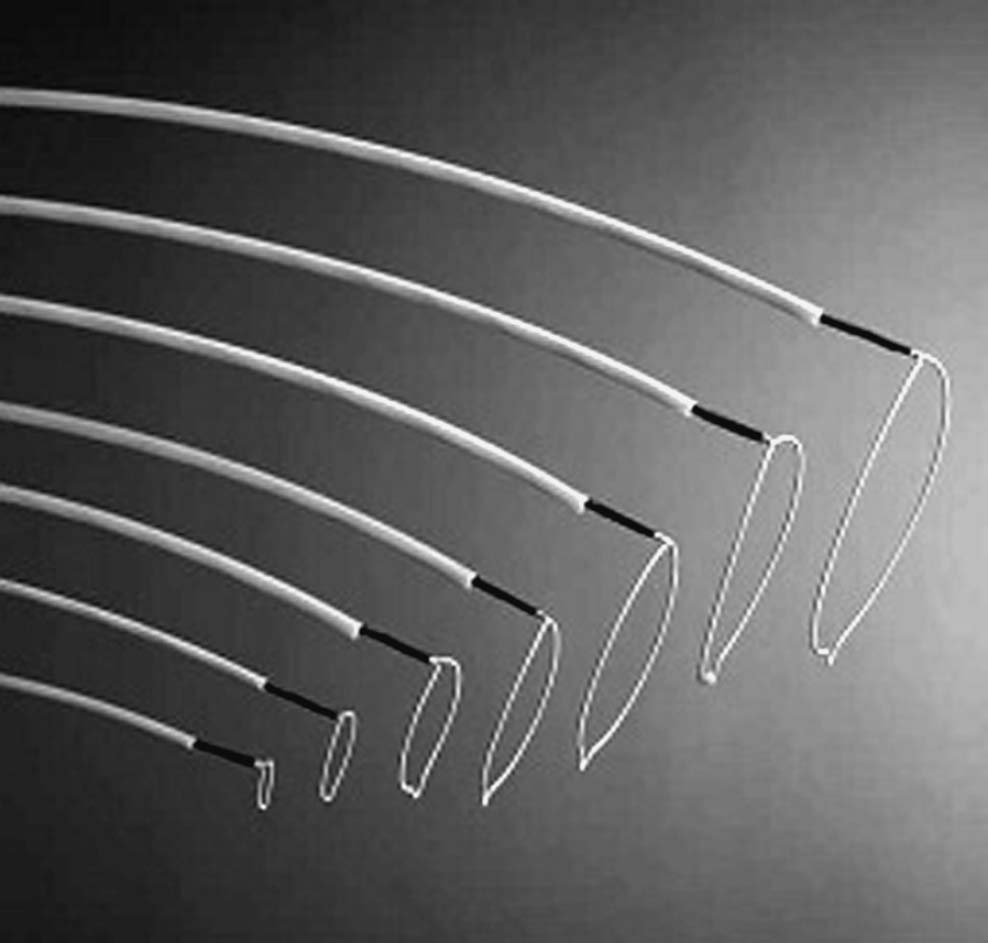
 Amplatz GooseNeck snare (loop size corresponding to clinical situation, up to 35 mm; Fig. 34.1)
Amplatz GooseNeck snare (loop size corresponding to clinical situation, up to 35 mm; Fig. 34.1)
– Diameter 1.32 mm (0.052 in.), length 120 cm, loop diameter variable
– Advantage: good visibility under fluoroscopy
– Disadvantage: poorer steerability with very soft and mobile snare or, for example,
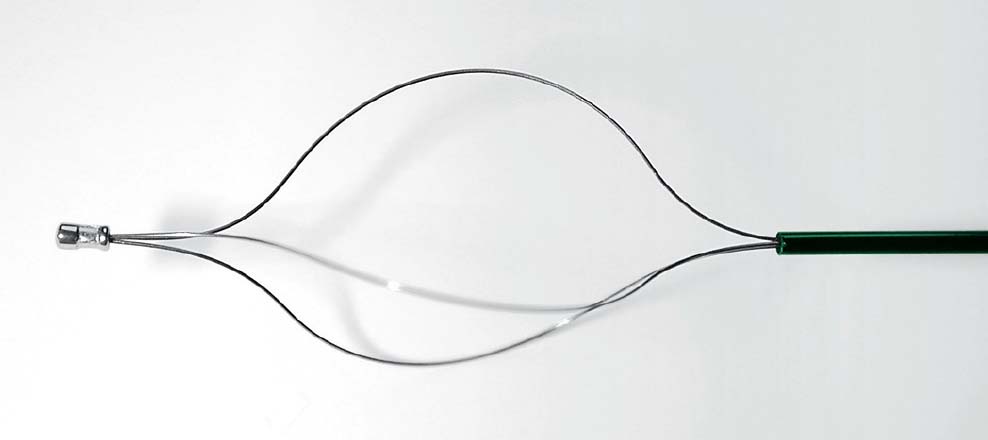
 Wire basket (e.g., with three wires, 10–15/20–25 mm; Figs. 34.2
Wire basket (e.g., with three wires, 10–15/20–25 mm; Figs. 34.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree