10 Percutaneous Coronary Interventions of Chronic Total Occlusions
PCI Strategy
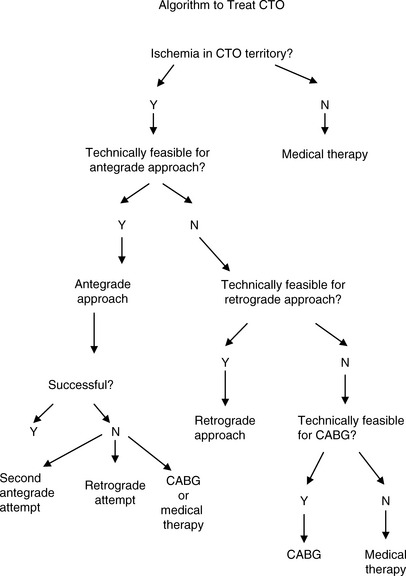
Prior to intervention, a formal strategy (“game plan”) should be devised (Fig. 10-1). By developing a game plan, overextending an already difficult procedure and increasing the risk of complications may be minimized. This plan must start with a decision as to whether the CTO is producing symptoms and/or ischemia, and if so, whether revascularization is actually required (as opposed to medical therapy). If revascularization is chosen, it must be decided whether the patient would be better served with CABG or PCI, as CTOs typically occur in patients with multivessel disease. If PCI is chosen, the next decision is whether the complexity is within the operator’s technical expertise or should be referred to a CTO super-specialist.
Favorable characteristics for the antegrade approach are shown in Figure 10-2 and listed in Table 10-1. Any combination of unfavorable characteristics significantly decreases the chance of success.
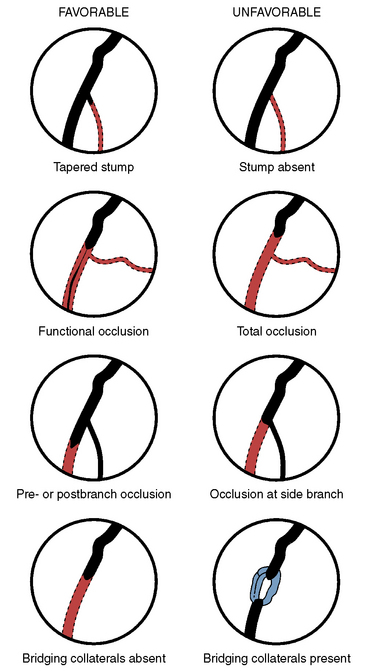
Figure 10-2 Morphology of total coronary occlusion: favorable and unfavorable morphology for procedural success.
(Modified from Safian RD, Freed M, Grines C, eds. The manual of interventional cardiology, 3 rd ed. Birmingham, MI: Physicians’ Press, 2001, p. 295.)
Table 10-1 Favorable and Unfavorable Characteristics for Antegrade Success for Chronic Total Occlusions
| Favorable |
| Unfavorable |
Technical Considerations for CTO PCI
Angiography
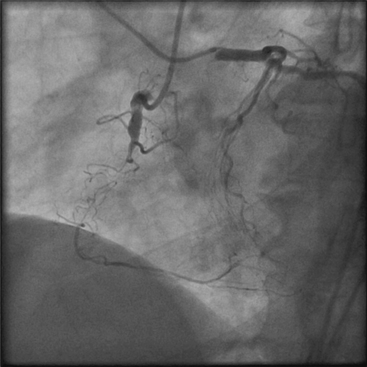
Excellent vessel opacification and knowledge of the occluded segment length and course are important factors for PCI success. Visualization of retrograde collateral filling of the target vessel is often essential. Bilateral coronary angiography is an invaluable aid in many CTO cases (Fig. 10-3). Using the antegrade approach, opacification through the target vessel may be insufficient to visualize the CTO and the course of the potentially recanalized channel. The contralateral vessel injection may allow for visualization of the vessel segment distal to the CTO. Administration of intravenous nitroglycerin may further improve visualization.
Antegrade Approach
Guide and Support Catheters
A guide catheter with good backup is extremely important. The diameter of the guide remains an operator choice. In general, the greater the backup required and the amount of hardware to be introduced into the vessel, the larger should be the catheter diameter. Although stand-alone guidewire passage across a CTO may be effective, support for wire passage is usually required. Support for guidewire passage can be obtained with end-hole microcatheter, e.g., Corsair (Fig. 10-5B) or small-diameter (1.25–1.5 mm) over-the-wire (OTW) balloon catheter and will increase the chance for wire passage through the total obstruction. Wire passage through a CTO into the true lumen increases the success rate to nearly that of a non-CTO, that is, > 90%–95%. Although passage of the wire distally through the true lumen is another major key for success, subintimal wire passage can still be effective.
CTO Guidewires
Wire choice is another key element to treatment success. There is a very large portfolio of available wires. In general, guidewires may be classified as hydrophilic and non-hydrophilic; Table 10-2 lists a few examples of each. Each wire has its own unique combination of flexibility, trackability, torque transmission (or steerability), lubricity (or hydrophilicity), shaft support, wire tip load or strength, wire tip prolapsibility, radiovisibility, ability to shape and retain tip configuration, tip taper and thickness, and tactile feedback. The operator should become familiar with the properties of each wire that might be applied to a lesion so that a wire plan can be developed.
Table 10-2 Examples of Equipment for Recanalization of Chronic Total Occlusion Using the Antegrade Approach
| Category | Example | Rationale for Use |
|---|---|---|
| Guiding catheter | Left: Amplatz, XB (Cordis), EBU (Medtronic), Voda (BSC) Right: Amplatz | Increased backup support |
| Guidewires | Hydrophilic wires: Fielder, Fielder XT (Asahi), Pilot 50 (Abbott) | Passage through microchannel |
| Increased tip load: Miracle Bros 3-12 (Asahi), Confianza Pro (Asahi) | Passage through “hard” proximal cap | |
| OTW balloon | 1.25–1.5 balloon diameter (multiple companies) | Increase wire force to proximal capPredilation after crossing CTO |
| Microcatheter | Corsair (Asahi), FineCross (Terumo, Tokyo, Japan) | Provide increased wire force to proximal cap |
| Tornus |