10 Percutaneous Coronary and Structural Heart Disease Interventional Techniques
The widespread use of percutaneous coronary and structural heart disease interventional techniques performed after diagnostic angiography for patients with ischemic and structural (e.g., valvular or atrial septal defects) heart disease is now commonplace. A companion book, the Interventional Cardiac Catheterization Handbook, expands on the concepts presented in this chapter and provides a more detailed foundation for indications, contraindications, and complications of interventional cardiology techniques. Table 10-1 lists diagnostic and therapeutic procedures performed in the catheterization laboratory.
Table 10-1 Diagnostic and Therapeutic Procedures in Cardiac Catheterization Laboratory
| Diagnostic Procedures | Therapeutic Procedures |
|---|---|
| Coronary angiography | Angioplasty—balloon stents, DCA |
| Ventriculography | Valvuloplasty |
| Hemodynamics | Shunt closure |
| Shunt detection | Thrombolysis |
| Ao and peripheral angio | Coil embolization |
| Pulmonary angio | Pericardiocentesis, window |
| Coronary hemodynamics | Percutaneous valve Rx |
| Endomyocardial biopsy |
Ao, angio; DCA, directional coronary atherectomy; Rx, treatment.
Percutaneous Coronary Interventions
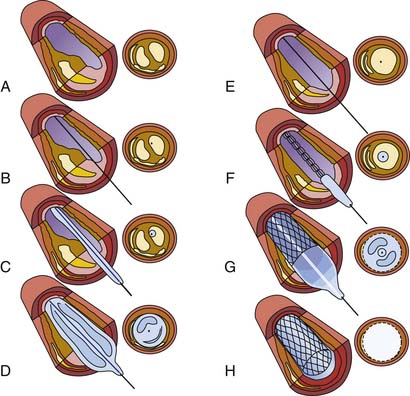
Figure 10-1 shows how to perform PCI. A guiding catheter is seated in the coronary ostium. A thin, steerable guidewire is introduced into the coronary artery and positioned across the stenosis into the distal aspect of the artery. An angioplasty catheter, which is considerably smaller than the guiding catheter, is inserted through the guiding catheter and positioned (in the artery) across the stenotic area by tracking it over the guidewire. The balloon or stent is on the PCI catheter. When the balloon or stent is placed correctly within the area to be treated, the balloon on the PCI catheter is inflated several times for periods ranging from 10 to 30 seconds. The inflation and deflation of the balloon stent in the blocked artery restores blood flow to an area of the heart previously deprived by the stenosed artery. After stent implantation and if no complications occur, patients usually stay overnight in the hospital and are discharged the following morning. Patients can usually resume their normal routine within several days.
How Balloon Angioplasty Works
Several theories regarding the mechanisms of angioplasty have been proposed.
Mechanism of Stents
The indications, contraindications, and complications of PCI are listed in Table 10-2.
Table 10-2 Indications, Contraindications, and Complications of Percutaneous Coronary Intervention (PCI)
Equipment
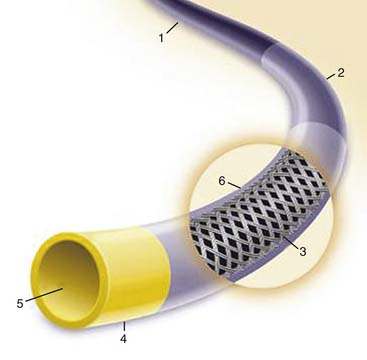
PCI equipment consists of three basic elements: the guiding catheter, the balloon-stent catheter, and the coronary guidewire (Fig. 10-2).
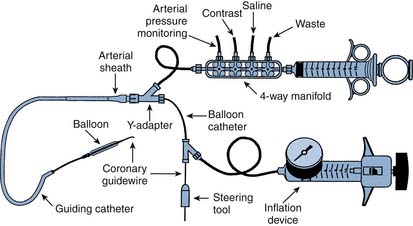
Figure 10-2 Diagram of components of percutaneous coronary intervention equipment.
(From Freed M, Grines C, Safian RD: The new manual of interventional cardiology, Birmingham, MI, 1996, Physicians’ Press.)
Guiding Catheter
A special large-lumen catheter is used to guide the coronary balloon catheter to the vessel that has the lesion to be dilated (Fig. 10-3). Compared with diagnostic catheters, guiding catheters have thinner walls and larger lumens, which allow contrast injections to be done while the balloon catheter is in place. The guiding catheters are stiffer than diagnostic catheters to provide support for advancing the balloon-stent catheters into the coronary artery. They respond differently to manipulation than diagnostic catheters. The guiding catheter tip is not tapered, occasionally blocking the ostium and causing pressure dampening while engaging the coronary ostium. A 6 F guiding catheter is generally used. Some catheters have relatively shorter and more flexible tips than other catheters, theoretically to decrease catheter-induced trauma. Others may have side holes to help maintain blood flow during PCI. Larger guiding catheters (7 F or 8 F) may be necessary for kissing balloons/stents, rotoblator burrs larger than 2 mm, and some cutting balloons. There are many different shapes of guiding catheters for different anatomic variations.
Functions of the Guiding Catheter
There are three major functions of a guiding catheter during PCI:
Balloon Catheters
Over-the-Wire (OTW) Angioplasty Percutaneous Coronary Intervention Systems
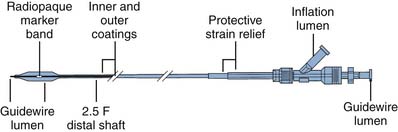
A standard OTW PCI catheter (Fig. 10-4) has a central lumen throughout the length of the catheter for the guidewire and a separate lumen for the balloon inflation. These catheters are approximately 145 to 155 cm long and can be used with long or short guidewires, usually 0.014 inch.
The advantages and limitations of OTW angioplasty balloon catheters are listed in Table 10-3. These catheters accept multiple guidewires, which allows for the exchanging of additional devices that may require stronger, stiffer guidewires. Maintenance of distal wire position beyond the target stenosis is paramount in coronary angioplasty. For OTW balloon catheters the guidewire can be extended to help maintain distal position while the balloon catheter is withdrawn completely over the guidewire to permit another balloon catheter to be exchanged and introduced over the same guidewire for additional dilations. A 300-cm exchange wire is also commonly used.
Table 10-3 Advantages and Limitations of Angioplasty Balloon Types
| Advantages | Limitations | |
|---|---|---|
| Over the wire | Distal wire position | Needs two people for exchange |
| Distal port for pressure, contrast injection | Accepts multiple guidewires | |
| Rapid exchange (monorail) | Ease of use Single-operator system | Needs good guide support |
| Enhanced visualization | Blood loss at Y valve during exchanging | |
| Poor balloon tracking | ||
| Fixed wire | Enhanced visualization | Lack of through lumen |
| Single-operator system | Exchanging balloon requires access to distal lesions and complete removal of balloon | |
| Use with small guiding catheters | Very low-profile PCI balloon |
OTW angioplasty balloon catheters have few limitations. A primary operator and experienced personnel are required to perform catheter exchanges. Several different types of devices can be used to fix a 155-cm guidewire in place to permit OTW catheters to be exchanged without using a 300-cm guidewire. These devices are now rarely used and have included a wire entangler, a balloon trapper, and a magnet fixation system (see later).
Rapid-Exchange (Monorail) Percutaneous Coronary Intervention Catheters
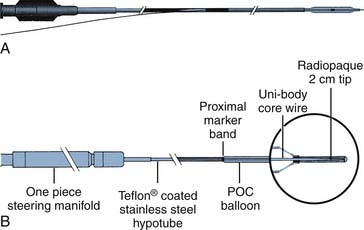
Rapid-exchange balloon catheters are the most popular catheters used today and were developed to allow a single operator to exchange the PCI catheters unassisted. This rapid exchange catheter differs from over the wire PCI catheters in that only a variable length of the shaft has two lumens (Fig. 10-5, A). One lumen is for balloon inflation and the other, which extends through only a portion of the catheter shaft, houses the guidewire. Because only a limited portion of the balloon requires dual lumens, the catheter shafts can be made smaller than over the wire systems.
Fixed-Wire Angioplasty Balloon Catheters
The fixed-wire catheter is rarely used today and has the balloon mounted on the wire with a distal flexible steering tip (Fig. 10-5, B). The proximal end of the catheter consists of a single, nonremovable port connected to a hollow metal tube (hypotube). A core wire extends from the hypotube to the end of the distal steerable tip. This assembly is coated with a thin plastic shaft that enhances flexibility. Fixed-wire balloons have only one enclosed lumen for balloon inflation.
The advantages and limitations of fixed-wire angioplasty balloon catheters are listed in Table 10-2. The small shaft size of the single-lumen design provides excellent coronary visualization. Because the balloon is mounted on the distal guidewire, the device can easily be used by a single operator. Fixed-wire balloon catheters are particularly useful for distal lesions, subtotal stenoses, and lesions located in tortuous small vasculature.