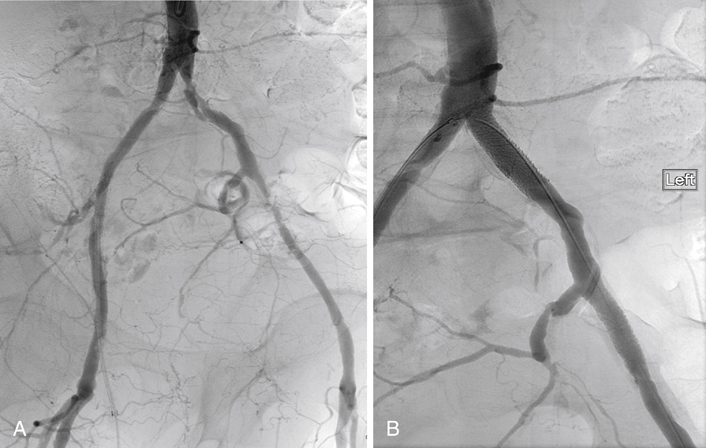
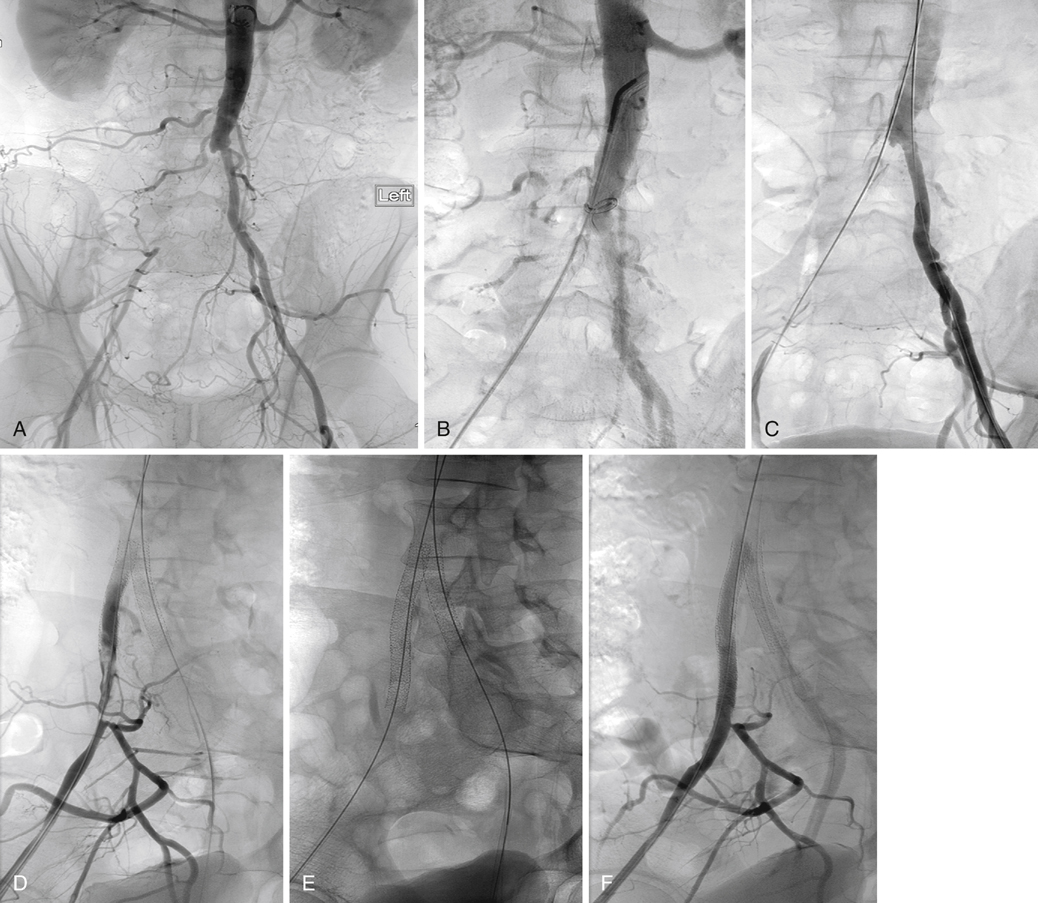
Endovascular treatment of AIOD should be considered for patients with disabling claudication or critical limb ischemia who have lesions with favorable expected results. The Trans-Atlantic Inter-Society Consensus (TASC) classification scheme, which stratifies patients into four groups according to the anatomic pattern of occlusive lesions, is useful to select patients for these interventions (Box 1). Patients with type A lesions (focal stenosis of the common or external iliac arteries) have the best results, and endovascular therapy is the treatment of choice for this group. Open surgical reconstruction is recommended for patients with the most severe pattern of disease (type D lesions). Comorbidities, patient’s preference, and the operator’s experience should be considered when choosing endovascular or open techniques for managing patients with types B and C lesions, with the majority of these patients currently treated with endovascular intervention. Endovascular interventions for common and proximal external iliac artery lesions are most easily performed through an ipsilateral retrograde femoral approach. If necessary or desirable, however, many interventions can be performed through a contralateral femoral puncture, with over-the-top contralateral access across the aortic bifurcation (Figure 1). Upper extremity vascular access is also technically feasible, but it is not preferred. Guidewire and catheter manipulations are more difficult over the longer working distance from the arm, and the larger-diameter sheath required for many interventional devices increases the likelihood of puncture site complications in the smaller arm vessels. Aortic lesions near its bifurcation should be considered complex lesions involving the distal aorta and both common iliac arteries. Safe and effective intervention in this situation typically requires the use of two balloons or stents, one in each iliac artery and projecting partway into the aorta so that they kiss in the distal aorta. Aortic lesions distant from the bifurcation or other critical branches are otherwise treated similarly to that described for iliac stenoses. Successful navigation of guidewires and catheters across the target lesion from the access site can require considerable skill and experience. Failure to achieve successful traversal is one reason for initial technical failure of the procedure. Navigation across a complete occlusion, with reentry into the true lumen of the vessel beyond the lesion, can be especially challenging. This maneuver is most often accomplished using angled hydrophilic guidewires and/or catheters (Figure 2). If reentry cannot be achieved from the chosen point of vascular access (e.g., ipsilateral common femoral), an attempt may be made from a new access site (e.g., contralateral common femoral or brachial). For more challenging cases, reentry devices such as the Outback (Cordis Corp., Bridgewater, NJ) or Pioneer (Medtronic, Fridley, MN) catheters can be used.
Percutaneous Arterial Angioplasty with and without Stenting for Atherosclerotic Aortic and Iliac Artery Occlusive Disease
Indications
Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
