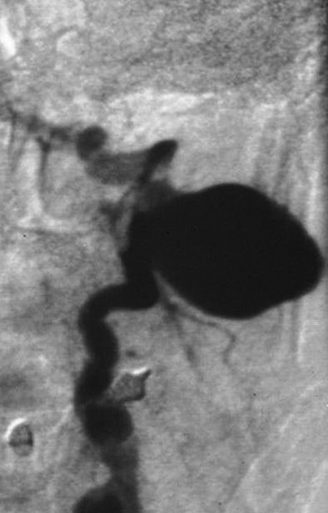
The most common vertebral artery injuries fall within one of two categories: blunt trauma of the neck, usually related to motor vehicle accidents, or iatrogenic injuries. A minority are secondary to firearms (Figure 1).
Systematic screening of patients with blunt neck injuries with magnetic resonance imaging (MRI) or computed tomography (CT) shows a high incidence of vertebral artery injury, with a majority of patients not experiencing clinical symptoms, but with a potentially high morbidity for those who develop signs of a stroke involving the vertebrobasilar territory.
From a practical standpoint, CT angiography (CTA) with multidetector machines is now considered a good screening modality for patients with acute cervical spine trauma. Angiography is still the most sensitive imaging technique to define vertebral artery injuries, but its invasiveness and risk in patients with severe head and neck injuries makes it an unlikely choice as a screening measure. MRI has been used in most prospective studies, but it is not universally available in areas that receive acute trauma patients. In addition, the fixation and life support devices in these patients interfere with MRI protocols. Nevertheless, MRI remains the best modality to detect early parenchymatous changes in the vertebrobasilar territory.
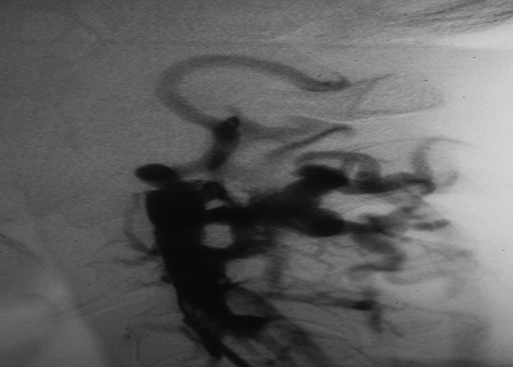
Patients undergoing systematic MRI studies following acute cervical spine trauma have a high incidence (20%–25%) of abnormalities in their vertebral artery, mostly occlusion and dissection, and 3% to 5% will develop a cerebellar or brain infarct, which is often lethal. The mechanism of injury in cervical spine trauma patients is usually distraction or compression of the artery, resulting in intimal flaps, dissections (Figures 2 and 3), pseudoaneurysms, or arteriovenous fistulas (Figure 4) of the vertebral artery. In a review of 1941patients with blunt trauma, the incidence of carotid or vertebral injury was 1.1%. Another extensive literature review reported that most patients with a vertebral artery injury have no clinical symptoms, but the few who develop a sudden deterioration after a brief normal neurologic interval have a morbid course.
In acute cervical spine trauma, the vertebral artery is injured along its transforaminal course, from C6 to C1. Vertebral artery injury occurs in 25% of patients with a fracture of the transverse process and in 35% of those with a facet dislocation. However, 20% of patients with acute cervical spine trauma sustain a vertebral artery injury in the absence of any identifiable bony fracture or dislocation. In these patients, the vertebral artery is injured by distraction–flexion and distraction–extension forces. A particularly worrisome course in patients with a history of cervical trauma is the development of stroke symptoms after several days, or even weeks, of neurologic clinical normality. This morbid course is the result of the progression to occlusion of the injured vertebral artery or its embolization into the basilar artery.
Vertebral artery injury associated with chiropractic manipulation of the neck falls into both blunt and iatrogenic categories of trauma. The attribution of vertebrobasilar stroke to the manipulation of the cervical spine has long been a subject of controversy. Although the incidence of vertebrobasilar stroke after chiropractic manipulation is low, its outcome is most serious: 52% develop a permanent neurologic deficit, and 5% to 18% die. The chiropractic literature states, on the basis of self-reporting, that the incidence of stroke following chiropractor manipulation is very small: between 1 per 1.3 million and 1 per 400,000 treatment sessions. However, a population-based study, using data from hospital admission codes for vertebrobasilar stroke and billing data for cervical spine manipulation, showed that the incidence was 1.3 per 100,000 cases of neck manipulation. Patients admitted with symptomatic vertebrobasilar occlusion or dissection were five times more likely than matched controls to have visited a chiropractor for cervical pain in the previous week.
In ascribing the vertebrobasilar stroke of a patient to a chiropractic manipulation one must also consider the fact that most patients go to a chiropractor because of neck pain, and the neck pain could have been the initial symptom of a spontaneous vertebral artery dissection. In that case the manipulation could have extended what was, till then, a limited dissection. Given the propensity for spontaneous dissection in patients with connective tissue disease, it seems sensible to advise them to avoid chiropractic manipulations.
Iatrogenic injuries of the V1 segment usually follow the placement of a central venous catheter. The most common lesion resulting from accidental puncture of a vertebral artery is a fistula either between the vertebral artery and the jugular vein or the vertebral artery and the vertebral vein. This injury is common because the vertebral vein is anatomically adjacent to the vertebral artery. The same mechanism just as often could result in an arteriovenous aneurysm.
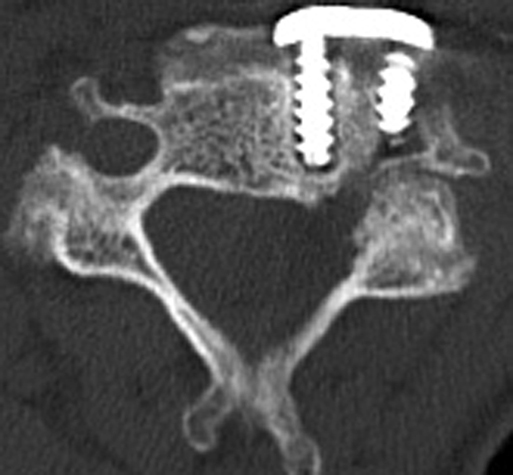
Anterior diskectomy seldom (0.3%–0.5%) results in vertebral artery injury in its intraspinal segment. When injury occurs it usually follows a lateral exploration or the drilling of an uncovertebral joint (Figure 5). It is easy to understand how this complication can occur when we observe in some patients the tortuosity and redundancy of their vertebral artery between the transverse processes. The vertebral artery is more likely to be injured during anterior cervical corpectomy. The favored technique for atlantoaxial fixation involves inserting a screw into the C1–C2 facet joint, and this maneuver carries a risk of 8% of lacerating the vertebral artery. In posterior cervical spine surgery, a rare vertebral artery injury is the perforation of the artery by the screw used for a plate fixation. Although spine surgeons have precisely defined the anatomic landmarks for safe drilling, variations in the course of the vertebral artery, including its extraforaminal excursions, are responsible for some of these infrequent injuries.
Only gold members can continue reading.
Log In or
Register to continue
Related


![]()