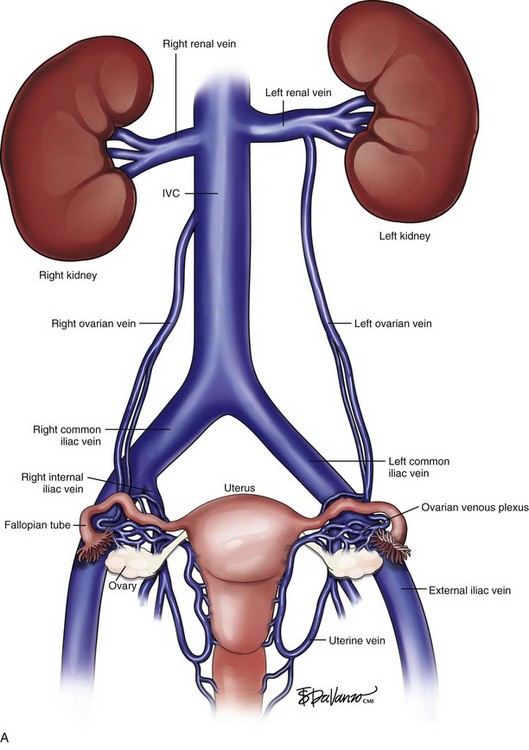
Chapter 17 Pelvic Congestion Syndrome and Ovarian Vein Reflux
Background
Pelvic congestion syndrome (PCS) is an underdiagnosed condition causing chronic pelvic pain. PCS was first described by Taylor in 1948,1 who described a number of specific patients suffering with pelvic pain; these patients had pelvic and ovarian varicosities from ovarian vein incompetence. Women with PCS are usually of menstruating age who report pelvic heaviness and pain that is aggravated by standing. They are typically multiparous and report that their symptoms worsen during the premenstrual period. These patients may also complain of dyspareunia.
Classification
As with many conditions there is a spectrum of pelvic venous syndromes that may affect patients. Scultetus et al.2 classified these patients into four types. Type 1 includes patients with limited vulvar varices. Patients with hypogastric vein reflux (including internal pudendal and obturator branches), usually with vulvar varicosities and hemorrhoids, represent type 2. Type 3 patients are diagnosed with gonadal vein obstruction due to a mesenteric aortic compression of the left renal vein (nutcracker syndrome). Type 4 patients have gonadal vein insufficiency that is characteristic of PCS. These patients may have lower extremity varicosities that originate in the pelvis and may also have associated hypogastric vein reflux.
Etiology
The cause of PCS is unknown and poorly understood. However, autopsy studies have found that a percentage of patients may have congenital absence of valves in the left ovarian vein.3 Interestingly, a significant number of patients (40%) with ovarian vein incompetence may remain asymptomatic. Additionally, the development of the incompetence and symptoms may be associated with mechanical stresses such as pregnancy as well as with certain hormonal effects.
Diagnosis
The diagnosis of this condition requires a significant clinical suspicion because there are many disorders that present with pelvic pain. The diagnosis for many years relied on clinical suspicion that would be confirmed at the time of direct venography. Additionally, a number of cases have been diagnosed with the discovery of pelvic varicosities at the time of laparoscopy. The use of transabdominal and transvaginal ultrasound has been described as a manner to diagnose PCS in a patient with pelvic pain4; however, its accuracy in widespread practice is limited. At present, when there is a clinical suspicion, the diagnosis is confirmed with either computed tomography venography (CTV) or magnetic resonance venography (MRV).5,6 MRV is the study of choice because of its lack of ionizing radiation and its ability to perform time-resolved imaging7 (Fig. 17-1).
Treatment
In the early years of the condition, surgical treatment consisted of surgical ligation of the ovarian vein. Recently there have been reports of laparoscopic ligations. Most commonly, percutaneous transcatheter treatment is used. Transcatheter treatment was first reported by Edwards in 1993,8 and these treatments have continued to adapt in technique over the years.
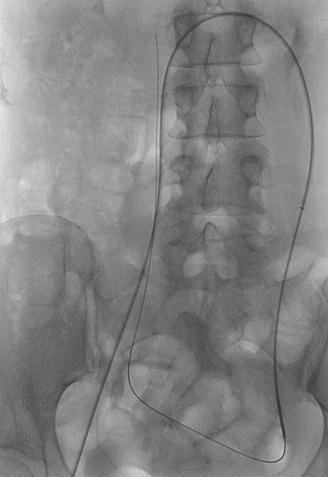
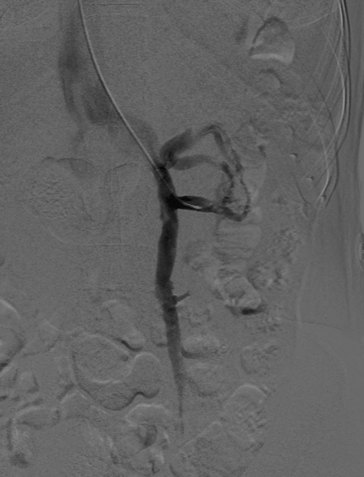
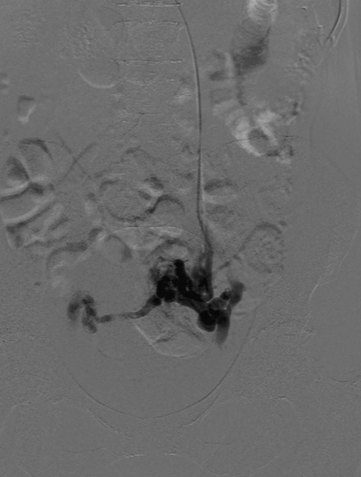
The percutaneous transcatheter treatment can be performed from either the femoral or jugular approach. We prefer the jugular technique as it allows a more natural angle into the left renal vein. Selection of the left as well as the right ovarian vein can be very difficult from the femoral approach because of the acute angle at the origin of the right ovarian vein with the inferior vena cava (Fig. 17-2). Injection of the left renal vein will usually depict the presence of a dilated (6 to 10 mm) left ovarian vein, which is incompetent (Fig. 17-3). There are usually cross pelvic collaterals filling the right ovarian venous system (Fig. 17-4). In a percentage of cases, the reflux causes filling of the internal iliac vein branches. Venography can be done during the Valsalva maneuver if the resting venogram does not demonstrate an enlarged ovarian vein.9 Additionally, the venogram can be repeated in a semierect position if a tilt table is available.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree