PEComatous Tumors
Marie-Christine Aubry, M.D.
Fabio R. Tavora, M.D., Ph.D.
Definition
PEComatous tumors encompass tumors thought to arise from perivascular epithelioid cells (PECs). PECs were first described in 1943 and are cells with variable morphology. The cells may be round to spindled and the cytoplasm variably clear to granular and eosinophilic. Similarly, the immunoprofile may be variable. By definition, PECs are positive for HMB45, melan-A, MART-1, and MITF. Expression of actin, estrogen (ER) and progesterone receptors (PR), and S100 protein tends to vary with the tumor type. In the lung, PEComatous tumors include lymphangioleiomyomatosis (LAM), clear cell tumor, angiomyolipoma, and a rare process often referred to as diffuse PEComatosis.1,2,3
Lymphangioleiomyomatosis
Clinical Findings
LAM constitutes <1% of cases of diffuse parenchymal lung disease. This disease affects predominantly women in reproductive age, with a mean age of 40 years at diagnosis, although it has also been described in postmenopausal women.4,5 LAM is associated with TSC and affects up to 40% of women with TSC.5,6 LAM is rarely reported in men, with only four biopsy-proven cases, three of whom likely had TSC.7
The most common presenting symptom is progressive dyspnea, followed by cough and hemoptysis.4,8 Complications associated with LAM include spontaneous pneumothorax in up to 70% of patients and lymphatic obstruction (chylothorax, chyloperitoneum, chylopericardium, and chyluria).4,5,8 Renal angiomyolipomas occur in 30% to 60% of patients with sporadic LAM4 and 93% of patients with TSC and LAM. Retroperitoneal and mediastinal lymphangioleiomyomas can also be seen along the lymphatic routes and with nodal involvement.4,9 Pulmonary function tests often show an obstructive or mixed pattern with increased gas volumes and reduced diffusing capacity, but a third of patients have a restrictive pattern or normal tests.4,5,10
Radiologic Findings
Radiologic findings include diffuse bilateral thin-walled cysts usually ranging from 0.2 to 2.0 cm in diameter on high-resolution chest computerized tomography scan (HRCT) (Fig. 71.1). Diffuse bilateral reticular infiltrates are seen in 80% of patients, pneumothorax in 30% to 40% of patients, and pleural effusion in 10% to 20% of patients. Hyperinflation is common.
Gross Findings
Grossly, LAM is characterized by diffuse bilateral cysts usually <2 cm in greatest dimension, but 10 cm in diameter cysts have been reported (Fig. 71.1).
Microscopic Findings
Histologically, thin-walled cysts are distributed throughout the lung. The walls of the cysts are lined by a nodular proliferation of cells (Fig. 71.2). Sometimes, it is difficult to appreciate the bundles of cells, which may appear inconspicuously at the cyst edges. LAM cells are variably round and epithelioid or spindled, with only minimal pleomorphism (Fig. 71.2). Nuclei are oval to cigar shaped, with fine to vesicular chromatin. Mitotic figures are rare. Cytoplasm is eosinophilic and moderately abundant and may show perinuclear vacuoles. LAM cells may infiltrate the blood vessels resulting in accumulation of hemosiderophages. In cases complicated by pneumothorax, the pleura may show reactive eosinophilic pleuritis. Lungs of patients with TSC may also show additional lesions including micronodular pneumocyte hyperplasia (MNPH) (Fig. 71.3), clear cell tumor, angiomyolipoma, and localized angiomyolipoma-like infiltrative lesions.1,11,12
The histologic findings of LAM are distinctive enough to confirm the diagnosis on a transbronchial biopsy, although they can be very subtle. Recognizing a smooth muscle cell proliferation distinct from the normal smooth muscle of vessels or airways is key and can be aided by immunostaining these cells with markers such as HMB45 and β-catenin, typically negative in normal smooth muscle.13
Ancillary Studies
Immunohistochemical studies show that LAM cells are usually strongly and diffusely reactive with antibodies to smooth muscle actin (SMA), desmin, and vimentin (Fig. 71.4). They can also be reactive
to ER and PR.14 The distinctive feature is immunoreactivity with HMB45 and MART-1 (melan-A), usually focal in the epithelioid LAM cells. β-catenin and cathepsin-κ are other useful diagnostic markers, shown to be more sensitive than HMB45 and ER/PR, and also specific when compared to entities that may enter the differential diagnosis of cystic lesions such as pulmonary Langerhans cell histiocytosis and emphysema.
to ER and PR.14 The distinctive feature is immunoreactivity with HMB45 and MART-1 (melan-A), usually focal in the epithelioid LAM cells. β-catenin and cathepsin-κ are other useful diagnostic markers, shown to be more sensitive than HMB45 and ER/PR, and also specific when compared to entities that may enter the differential diagnosis of cystic lesions such as pulmonary Langerhans cell histiocytosis and emphysema.
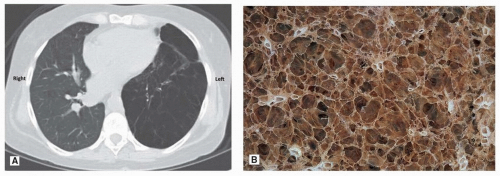 FIGURE 71.1 ▲ Lymphangioleiomyomatosis. A. Chest tomography of patient with LAM post single right lung transplantation. The right lung is radiologically normal. In contrast, the left lung shows innumerable thin-walled cysts filled with air. B. The gross highlights the numerous thin-walled cysts distributed throughout the lung parenchyma.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|