and Alessandra Cancellieri2
(1)
Department of Radiology, Bellaria Hospital, Bologna, Italy
(2)
Department of Pathology, Maggiore Hospital, Bologna, Italy
Radiology | Giorgia Dalpiaz | |
Pathology | Alessandra Cancellieri |
Alveolar pattern | Definition | Page 146 |
Alveolar key signs | Ground-glass opacity Consolidation | Page 147 Page 147 |
Ancillary signs | Hypodense consolidation Hyperdense consolidation Cystic consolidation Crazy paving Head-cheese sign Reversed halo sign (atoll sign) Perilobular opacities Lobular/sublobular opacities Tree-in-bud sign, bronchiolar | Page 149 Page 150 Page 151 Page 152 Page 153 Page 154 Page 155 Page 156 Page 157 |
Subset acute and table | Page 160 | |
Subset chronic and table | Page 161 |
Alveolar Pattern
Definition
An alveolar pattern is defined by the existence of more or less broad portions of the lung more opaque than normal due to partial or complete alveolar filling. With a few exceptions, the pulmonary architecture is overall preserved, and, if signs of interstitial involvement are present, they are not prevalent. On HRCT the different opacity of the alveolar pattern reminds the variable density of the clouds.
Air-space-filling pattern, cloudy opacities
Why are some clouds white and others gray? The color depends on a physical characteristic called reflectance, which indicates the percentage of light that is reflected from the cloud. In general, denser clouds have a reflectance of 90 % and are thus light in color.
In alveolar diseases, this pattern is predominant; however, there are other diseases in which alveolar opacities may be found, albeit less important or sporadic. They are therefore described in the relevant chapters.
The HRCT key signs are:
Ground-glass opacity
Consolidation
The ancillary signs are:
Hypodense consolidation
Hyperdense consolidation
Cystic consolidation
Crazy paving
Head-cheese sign
Reversed halo sign (atoll sign)
Perilobular pattern
Lobular/sublobular consolidation and GGO
Tree-in-bud sign, bronchiolar
The prevalent distribution of the signs, together with the presence of non-parenchymal signs, may be helpful for the diagnosis of a specific disease (please see the tables at the end of this chapter).
Alveolar Key Signs
Ground-Glass Opacity (GGO)
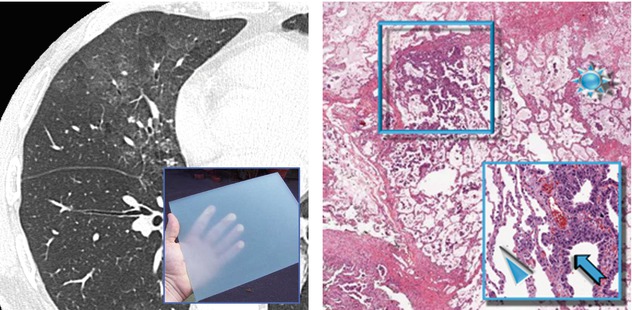
On CT scans, ground-glass opacity (GGO) appears as hazy increased opacity of the lung, with preservation of bronchial and vascular margins. Ground-glass opacity is less opaque than consolidation, in which bronchovascular details are obscured. The final effect is similar to the ground glass inserted in windows and doors (please see the left image below).
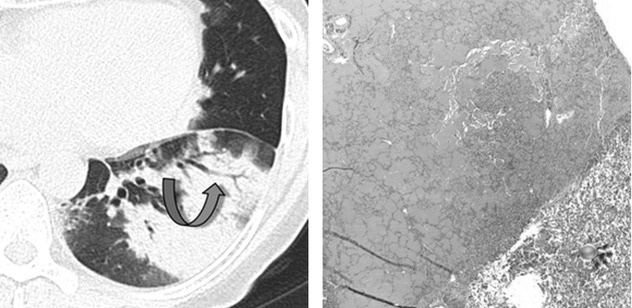
Pathologically, it may be caused by partial filling of air spaces and/or interstitial (mainly, alveolar septal) thickening due to fluid and/or cells. An example, illustrated in the figures below, is mucus in pneumonia-like pattern of mucinous adenocarcinoma. There are both a diffuse partial filling of air spaces due to mucus () and the lepidic growth of the neoplasm along alveolar septa (⃞). In the close-up, note the comparison between the different thickening of the normal alveolar septa (►) and the pathological ones (➨). Please also refer to the chapter entitled “Thinking Through Pathology”.
GGO
GGO may also be due to partial collapse of alveoli, increased capillary blood volume, or a combination of these, the common factor being the partial displacement of air.
GGO may also be due to interstitial fibrosis. It is variously associated with traction bronchiectases and bronchiolectases, fibrotic reticular abnormalities, and volume loss (please also refer to chapter “Fibrosing Pattern”).
Dark bronchogram sign (“overly good” visualization of bronchial structures within areas of ground-glass opacity) is a helpful mark to recognize minimal diffuse GGO.
GGO can be seen in all patients with an underlying alveolar lung disease, so its diagnostic value in isolation is limited; however, the clinical context (acute or chronic), together with the distribution and in combination with associated signs, may be helpful (please see the tables at the end of this chapter).
Engeler CE (1993) Ground-glass opacity of the lung parenchyma: a guide to analysis with high-resolution CT. AJR Am J Roentgenol 160(2):249
Hansell D (2008) Fleischner Society: glossary of terms for thoracic imaging. Radiology 246(3):697
Miller WT Jr (2005) Isolated diffuse ground-glass opacity in thoracic CT: causes and clinical presentations. AJR Am J Roentgenol 184(2):613
Consolidation
Consolidation appears as a homogeneous increase in pulmonary parenchymal attenuation that obscures the margins of vessels and airway walls. An air bronchogram may be present ( ).
).
 ).
).Pathologically, consolidation is due to a complete filling of alveoli by any material (exudate, cells, or other disease product can cause a similar radiological aspect) – the common factor being the full displacement of air from alveoli. An example, illustrated in the figure below, is pulmonary alveolar proteinosis (PAP). Note the abrupt transition between the area in which alveoli are filled by proteinaceous material and the normal lung (). Please also refer to the chapter entitled “Thinking Through Pathology >Pattern >Alveolar Filling.”
Consolidation can be seen in all patients with an underlying alveolar lung disease, so its diagnostic value by itself is limited; however, the clinical context (acute or chronic) and the distribution may be helpful together with the associated signs (please see the tables at the end of this chapter).
Hansell D (2008) Fleischner Society: glossary of terms for thoracic imaging. Radiology 246(3):697
Ancillary Signs
Hypodense Consolidation
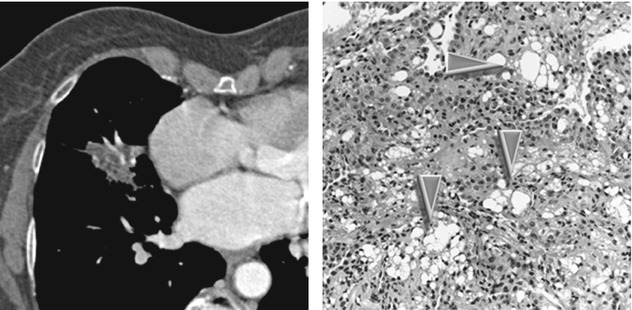
Using mediastinal window, an attenuation of consolidation is defined hypodense when it is lower than the muscle. It may be visible on CT after intravenous contrast material administration (please see CT image below). Sometimes the hypodense consolidation may be visible on unenhanced CT (HRCT) due to very low-density material (e.g., fat ► in lipoid pneumonia). Hypodense consolidations can result from ischemia (lung infarction) or from the presence in the air space of mucinous neoplasms (primary or metastatic mucinous adenocarcinoma), mucus (obstructive pneumonia with abundant accumulation of secretions), necrosis (necrotizing pneumonia), or fat (lipoid pneumonia, see the images below). With the exception of infarct, on enhanced CT you can also find the so-called angiogram sign, i.e., the visualization of pulmonary vessels within an airless, low-attenuation consolidation (please see CT image below). Please also refer to angiogram sign in “Case-Based Glossary with Tips and Tricks”.
Low-attenuation consolidation, low-density consolidation
Fat-containing hypodense consolidation shows CT-negative Hounsfield units (values between −150 and −30 HU).
Hypodense consolidation is recognizable only with CT mediastinal window, and it is more visible on contrast enhancement CT (see the figure above).
Diseases with hypodense consolidation:
Lipoid pneumonia: fatty consolidation (−150 and −30 HU) with dependent distribution (please see the figures above); patchy GGO and crazy paving often coexist.
Mucinous adenocarcinoma, primary or metastatic: low-density consolidation with possible air-filled cystic spaces (please also refer to bubble-like sign in “Case-Based Glossary with Tips and Tricks”); patchy GGO often coexists.
Obstructive pneumonia: crucial is the visibility of abundant accumulation of secretions inside the airways.
Lung infarction: contrast enhancement CT shows filling defects within the pulmonary vasculature with acute pulmonary emboli.
Necrotizing pneumonia: progression to a necrotizing pneumonia can occur from either virulence factor of the microorganism, predisposing factors of the host, or both. It can result from a large number of pathogens, mostly bacteria. Normal pulmonary parenchymal architecture within the necrotic segments is often lost.
MRI with “water-sensitive” sequences is useful in the diagnosis of patients with pulmonary consolidations suspected to be mucinous adenocarcinoma.
Betancourt SL (2010) Lipoid pneumonia: spectrum of clinical and radiologic manifestations. AJR Am J Roentgenol 194(1):103
Gaeta M (2012) MRI differentiation of pneumonia-like mucinous adenocarcinoma and infectious pneumonia. Eur J Radiol 81(11):3587
Hyperdense Consolidation
Attenuation higher than the muscle seen as dense/calcified diffuse or focal pulmonary opacities can result from a variety of different conditions. They can be due to deposition of calcium or, less commonly, other high-attenuation material such as talc, amiodarone, iron, mercury, iodinated substances, and barium sulfate.
Small and focal, hyperdense opacities inside a consolidation can be secondary to dystrophic calcifications in previously damaged lung parenchyma or, most commonly, as a result of infection diseases (►).
High-attenuation consolidation, calcified consolidation
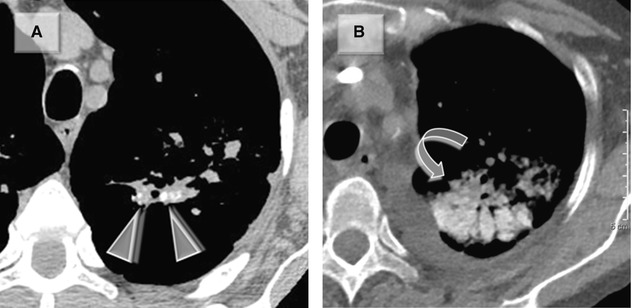
Diseases with multiple small focal hyperdense opacities inside the consolidation (Figure A above):
Tuberculosis: parenchymal focal calcifications are frequently seen in tuberculosis (►). A sequela of dystrophic calcification follows caseation, necrosis, or fibrosis. These nodules are seen as well-circumscribed parenchymal calcifications with fibrosis. Most patients with pulmonary nodular calcifications secondary to tuberculosis are located in the upper lobes and the upper segments of lower lobes. Calcified hilar or mediastinal lymph nodes often coexist.
Amyloidosis: the diffuse parenchymal pattern is mostly nodular and septal, although patchy consolidations may be seen. Basal and peripheral distribution is the dominant aspect. Areas of consolidations could show calcifications, some of them with punctate aspect. Lymph node enlargement, together with unilateral or bilateral pleural effusions, may be associated findings.
Calcified atelectasis: chronic atelectasis can be rarely seen as calcified consolidation, often with gravity-dependent distribution.
Silicoproteinosis: it may have focal calcifications, usually seen as small punctate calcified foci inside the areas of consolidation. This disease can also show hyperdense, often perihilar masses. Conglomerate masses are usually oval and have irregular borders.
Diseases with diffuse hyperdense consolidation (Figure B above):
“Metastatic” pulmonary calcification (MPC): HRCT findings are characterized by high-attenuation consolidtations ( ) most marked in the upper zones. Nodules which may contain foci of calcification may coexist.
) most marked in the upper zones. Nodules which may contain foci of calcification may coexist.
Drug toxicity (amiodarone): the association of dense lung air-space consolidations with high density of the liver and spleen is characteristic of amiodarone impregnation. Consolidations are usually peripheral in location. High-attenuation nodules or masses sometimes coexist.
Pulmonary alveolar microlithiasis: it is a rare chronic disease characterized by widespread calcific intra-alveolar concretions within alveolar spaces. In patients with long-standing disease, numerous adjacent hyperdense nodules result in areas of high-attenuation consolidation. Clinical symptoms are usually absent and, when present, are characterized by dyspnea on exertion.
Talcosis: in the late stage of the disease, hyperdense consolidations or confluent perihilar masses may be present. These lesions are similar to those seen in progressive massive fibrosis caused by silicosis.
Marchiori E (2005) Diffuse high-attenuation pulmonary abnormalities: a pattern-oriented diagnostic approach on high-resolution CT. AJR 184:273
Chan E (2002) Calcium deposition with or without bone formation in the lung. Am J Respir Crit Care Med 165:1654
Cystic Consolidation
Cysts (black holes) inside the consolidations and the GGO may be large or small, rounded, oval or serpentine, and sometimes confluent.
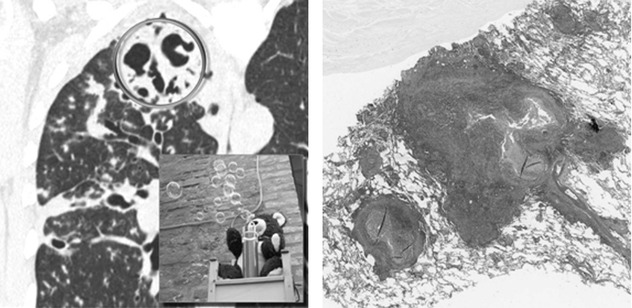
Pathogenesis: true cavitation (more often round or oval, e.g., TB – please see the HRCT  and histologic images below), pseudo-cavitation (bubble-like lucencies following bronchiolar obstruction due to a check-valve mechanism), and air bronchiologram (serpentine or linear in shape due to ectatic phenomena)
and histologic images below), pseudo-cavitation (bubble-like lucencies following bronchiolar obstruction due to a check-valve mechanism), and air bronchiologram (serpentine or linear in shape due to ectatic phenomena)
 and histologic images below), pseudo-cavitation (bubble-like lucencies following bronchiolar obstruction due to a check-valve mechanism), and air bronchiologram (serpentine or linear in shape due to ectatic phenomena)
and histologic images below), pseudo-cavitation (bubble-like lucencies following bronchiolar obstruction due to a check-valve mechanism), and air bronchiologram (serpentine or linear in shape due to ectatic phenomena)Bubble‐like lucencies
Nonneoplastic diseases with cystic consolidation:
Infection (e.g., TB): the presence of cavitated consolidations or nodules in the apical and posterior segments of the upper lobes and/or the superior segments of lower lobes (please see the images above) is suggestive of TB. Another hallmark is hilar/mediastinal lymphadenopathy with possible central necrosis, more visible on contrast enhancement CT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


