Pathway for the Management of Survivors of Out-of-Hospital Cardiac Arrest, Including Therapeutic Hypothermia
Eyal Herzog
Eitan Klein
Emad F. Aziz
Janet M. Shapiro
Cardiovascular disease (CVD) is the leading cause of death in the United States. Mortality data show that CVD as the underlying cause of death accounts for 35.3% of all deaths in the United States.1 There is a wide variation in the reported incidence and outcome of out-of-hospital cardiac arrest (OHCA). Cardiac arrest is defined as cessation of cardiac mechanical activity with absence of signs of circulation. The estimated number of OHCA cases is approximately 300,000 per year in the United States.1 The median reported survival to hospital discharge after OHCA with any first reported rhythm is 7.9%.1
Two landmark studies published together in 2002 demonstrated that the use of therapeutic hypothermia after cardiac arrest decreased mortality and improved neurological outcome.2,3 Based on these studies, the International Liaison Committee on Resuscitation and the American Heart Association recommended the use of therapeutic hypothermia after cardiac arrest.4,5
Therapeutic hypothermia is defined as a controlled lowering of core body temperature to 32°C or up to 34°C. This temperature goal represents the optimal balance between clinical effect and cardiovascular toxicity.6 Therapeutic hypothermia requires resources to implement—including device, close nursing care, and monitoring. It is important to select patients who have potential for benefit from this technique, which is a limited resource and carries potential complications. A collaborative team approach involving physicians and nurses is critical for successful development and implementation of this kind of protocol.7
This pathway is limited to OHCA and does not include inhospital arrest.
PATHWAY DESCRIPTION
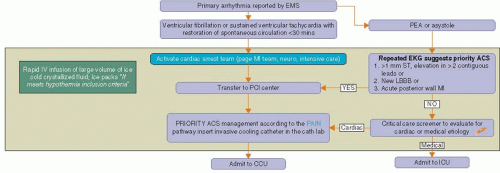
The pathway is divided into three steps as shown in Figure 20.1.
Step I. From the field through the emergency department (ED) into the cardiac catheterization laboratory and to the critical care unit.
Step II. Induced invasive hypothermia protocol in the critical care unit.
Step III. The management following the rewarming phase including the recommendation for out-of-hospital therapy and the ethical decision to define goals of care.
STEP I
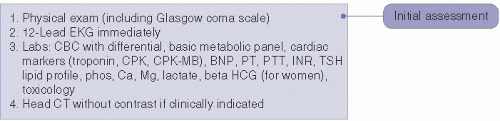
Presentation to the emergency department, proceeding to the cardiac catheterization laboratory and to the critical care unit. Upon arrival of a survivor of OHCA to the ED, the initial assessment (Figure 20.2) includes vital signs, physical examination, and neurologic examination with Glasgow coma score. Immediate 12-lead EKG is obtained and laboratory testing performed.
Initial laboratory testing includes complete blood count (CBC) with differential, basic metabolic panel, cardiac marker (troponin, CPK, CPK-MB), B-type natriuretic peptide (BNP), prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR), lipid profile, phosphorus, calcium, magnesium, lactate, β-HCG (for women), TSH, and toxicology screening. We recommend a head CT without contrast only if it is clinically indicated and will not delay transfer to the cardiac catheterization laboratory.
The patient is stabilized in the ED where antiarrhythmic and vasopressor therapy may be administered, in addition to ventilator support.
The ED physician receives the emergency medical services (EMS) report of the primary rhythm and duration of cardiopulmonary resuscitation (CPR). This reported arrhythmia is the key decision point in our pathway.
The prognostically important distinction is between patients with documented ventricular fibrillation (VF) or sustained ventricular tachycardia (VT) who had a restoration of spontaneous circulation (ROSC) in <30 minutes and patients with reported asystole or pulseless electrical activity (PEA) (Figure 20.3).
If the initial rhythm was VF or VT with an ROSC of ≤30 minutes the cardiac arrest team is activated, and the patient will proceed to the cardiac catheterization laboratory (Figure 20.4).
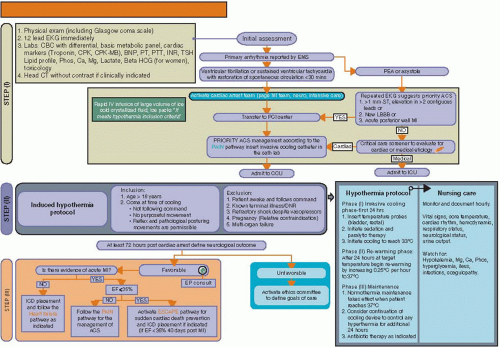
Figure 20.1. The comprehensive pathway for the management of survivors of out-of-hospital cardiac arrest.
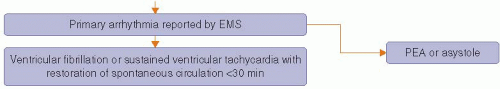
Figure 20.3. Identification of the primary arrhythmia that led to the cardiac arrest. PEA pulseless electrical activity.
If the initial reported arrhythmia was PEA or asystole, the next step will depend on the EKG performed in the ED (Figure 20.4). If the EKG performed in ED is suggestive of priority ACS (including ST elevation MI, left bundle branch block, or acute posterior wall MI), the MI team should be activated, and the care is similar to those patients with reported VF or VT arrest.
If priority EKG findings are not seen but the etiology of the arrest is most likely owing to primary cardiac disease, the cardiology fellow will admit the patient to the cardiac care unit. We recommend an emergency echocardiogram.
If the etiology is likely noncardiac, the patient will be admitted to the medical intensive care unit.
The cardiac arrest team includes the following 10 people.
The traditional (acute coronary syndrome) ACS-MI team comprises the following members10:
Interventional cardiologist on-call-the team leader
CCU director
Cardiology fellow on-call
Interventional cardiology fellow on-call
Cath lab nurse on-call
Cath lab technician on-call
CCU nurse manager on-call In addition the following personnel form the team:
The neurologist on-call
9. The critical care attending on-call and
10. The medical resident screener
The MI team is activated by a single page to the central call center by the ED physician.
Steps in the emergency department.
Decision to initiate induced hypothermia is made jointly by the ED physician and the cardiology or critical care physician. It is very important to review the hospital center’s inclusion and exclusion criteria and decide whether the patient is a candidate for the therapeutic hypothermia protocol (Figure 20.5).
The physician places an order to initiate hypothermia protocol.
Noninvasive hypothermia is initiated by the administration of iced saline in ED.
Our goal is to transfer the patient to the PCI center as soon as possible with a target door-to-balloon time of <90 minutes.
The management of the patient at this point is according to our Priority risk, Advanced risk, Intermediate risk, and Negative/low risk (PAIN) pathway following the priority ACS algorithm.10
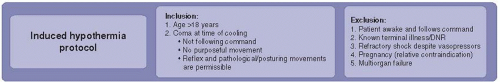 Figure 20.5. Inclusions and exclusions criteria for patients who are candidate for the therapeutic hypothermia protocol. |
A detailed description of this pathway appears in Chapter 1 of this book.
Following cardiac catheterization, several steps occur while the patient is still in the catheterization laboratory:
The femoral arterial sheath is maintained as an arterial catheter, which is necessary to obtain blood pressure readings and arterial blood gas analyses.
The intravascular hypothermia catheter is inserted under strict aseptic technique.
All patients are then transferred from the catheterization laboratory to the CCU where invasive hypothermia is initiated.
STEP II
Induced invasive therapeutic hypothermia protocol in the critical care unit.




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree