Pathologic Changes Involving Alveolar Septa and Interstitium
Allen P. Burke, M.D.
Fabio R. Tavora, M.D., Ph.D.
Inflammation
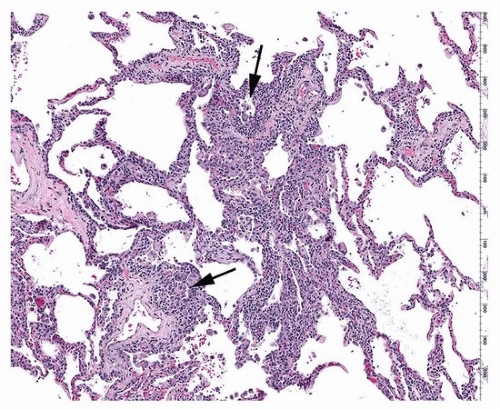
The most common type of inflammation in the alveolar septa is a mixture of mononuclear cells, including lymphocytes (usually predominantly T cells), macrophages, and plasma cells. If a pattern is recognizable, it is important to mention if it appears bronchiolocentric (Figs. 2.1 and 2.2) or perivascular (Fig. 2.3). There is often reactive pneumocyte hyperplasia, which indicates organizing lung injury of various causes and stages. The organizing lung injury may show discrete areas of organizing pneumonia.
The differential diagnosis of chronic interstitial pneumonitis (a nonspecific pattern of diagnosis) is outlined in Table 2.1.
Neutrophilic inflammation is less common and may be seen in infection (Fig. 2.4) and in areas close to an infarction. It is a hallmark of autoimmune injury (capillaritis, Fig. 2.5) and may be seen in alloimmune injury as well (antibody-mediated rejection).
Other components of interstitial inflammation may include eosinophils, seen in allergic or in eosinophilic pneumonia and to a lesser degree in hypersensitivity pneumonitis.
Fibroblasts and Collagen
Chronic inflammation may progress to interstitial fibrosis in a variety of settings, including interstitial pneumonias, organizing lung injury, and hypersensitivity pneumonitis. Initially, there are fine strands of collagen in a cellular matrix (Fig. 2.6), which may become more collagenized or form localized areas with organizing pneumonia (Fig. 2.7). Type II pneumocyte hyperplasia is typical when there is early collagen
deposition. Denser collagen may occur with organizing diffuse alveolar damage (Fig. 2.8) or smoking-related fibrosis. Dense acellular collagen, often with “naked” granulomas, is typical of sarcoidosis, although the scarring is not typically within alveolar capillaries.
deposition. Denser collagen may occur with organizing diffuse alveolar damage (Fig. 2.8) or smoking-related fibrosis. Dense acellular collagen, often with “naked” granulomas, is typical of sarcoidosis, although the scarring is not typically within alveolar capillaries.
Elastosis
Elastosis is an extremely common finding especially in localized reactions to tumors and pneumothorax. Caps of elastosis in the apices (“apical caps”) are present in most lungs of older people. When diffuse, the term “pleuroparenchymal fibroelastosis” is used. Elastosis does not typically demonstrate an alveolar septal distribution but is associated with alveolar collapse and loss of normal architecture.
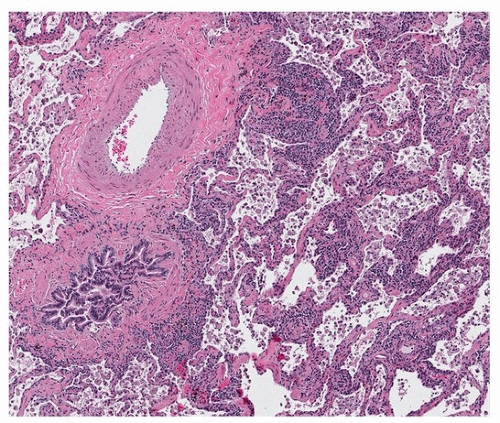 FIGURE 2.2 ▲ Chronic interstitial inflammation, peribronchiolar. There is a large bronchovascular bundle on the left. The ultimate diagnosis was probable hypersensitivity pneumonitis. |
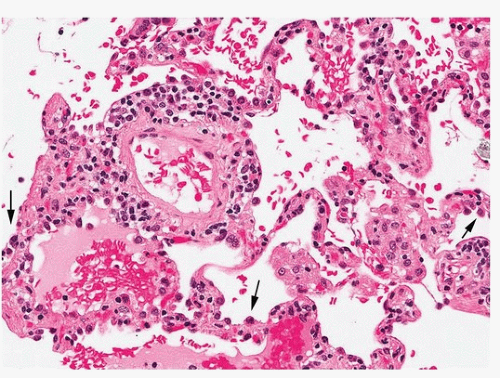 FIGURE 2.3 ▲ Chronic interstitial inflammation interstitial and perivascular. There is mild reactivity to alveolar lining cells (arrows). The patient had an undifferentiated connective tissue syndrome and interstitial cellular infiltrates that responded to steroids. The clinicopathologic diagnosis was interstitial pneumonia associated with rheumatoid arthritis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|