Pathologic Changes in Pulmonary Vessels
Allen P. Burke, M.D.
Joseph J. Maleszewski, M.D.
Arterial Changes, Elastic Pulmonary Arteries
Thromboembolism
Thrombus within the central pulmonary arteries is typically related to embolic phenomena and is most frequently seen at autopsy. Recurrent pulmonary embolism (chronic thromboembolic pulmonary disease) may cause “narrowing” of the pulmonary trunk and main pulmonary arteries and sometimes requires endarterectomy and surgical excision. Rarely, in situ thrombosis may be present due to atherosclerosis, vasculitis, or a pulmonary artery malignancy.
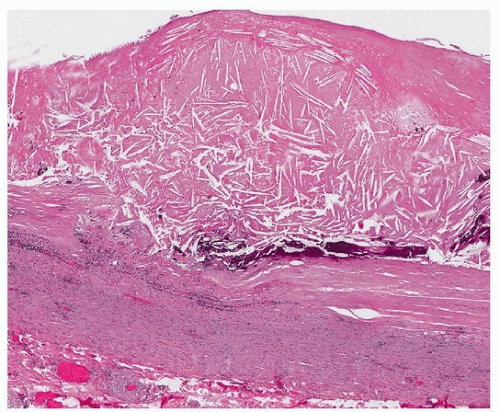
Atherosclerosis
The pulmonary circulation is resistant to the development of atherosclerosis, probably secondary to the different pressures and hemodynamics when compared to the systemic circuit. The exception to this rule occurs in patients with pulmonary arterial hypertension (PAH), who may develop typical features of atherosclerosis, including lipidrich atheromas (Fig. 8.1). Typically, there is associated dilatation of the pulmonary artery in addition to atheroma in the setting of pulmonary arterial hypertension. There will invariably be other long-standing changes of pulmonary hypertension, including right ventricular hypertrophy and other findings of cor pulmonale. Pulmonary arterial atherosclerosis is essentially a diagnosis made at autopsy.
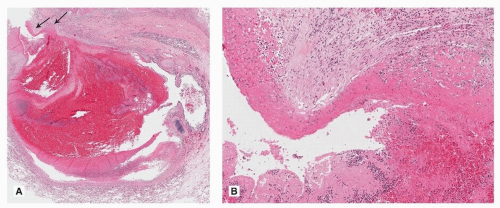
Arteritis
Vasculitis of the main pulmonary arteries is rare. Takayasu disease may involve the proximal pulmonary circulation, although much less frequently than the aorta. The histologic findings are similar to that seen in the aorta and its branches. Typically, this includes a granulomatous medial infiltrate, with intimal and adventitial fibrosis. Necrotizing arteritis may rarely occur in patients with Behçet disease (Fig. 8.2).
Pulmonary Arterial Dissection
Spontaneous dissection of the proximal pulmonary arteries is a rare complication of severe, chronic arterial pulmonary hypertension of any cause. The main pulmonary artery is usually the site of involvement, and extension to the branch arteries is uncommon. Rare reports of dissection occurring as a complication of aneurysm formation (caused by infection, trauma, or connective tissue diseases) have been reported. Rupture of the dissection may occur, leading to hemopericardium and/or tamponade.
Arterial Changes, Muscular Pulmonary Arteries
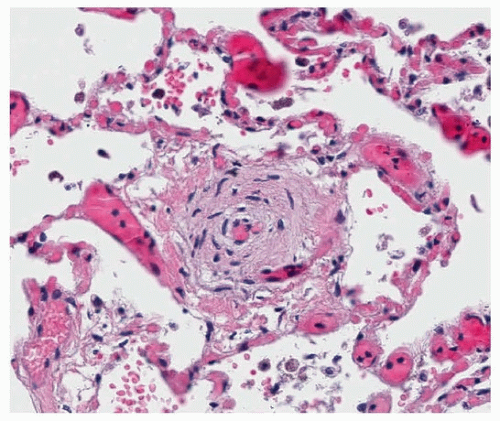
Muscularization of Arterioles
Muscularization of arterioles, proximal to the alveolar capillary bed, is a feature of persistent pulmonary hypertension of the newborn (Fig. 8.3) (see Chapter 13).
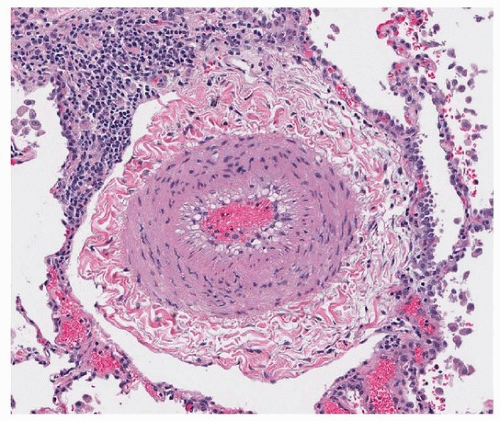
Medial Hypertrophy
Medial hypertrophy of pulmonary arteries is defined as a medial thickness >10% of the diameter (or 20% if both sides are measured) (Fig. 8.4). Medial hypertrophy is nonspecific and may be present in pre- and postcapillary causes of pulmonary hypertension. Thickened small muscular arterial branches may occur in the periphery, especially as a reaction to interstitial lung process, and are not necessarily reflective of increased arterial pressures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree