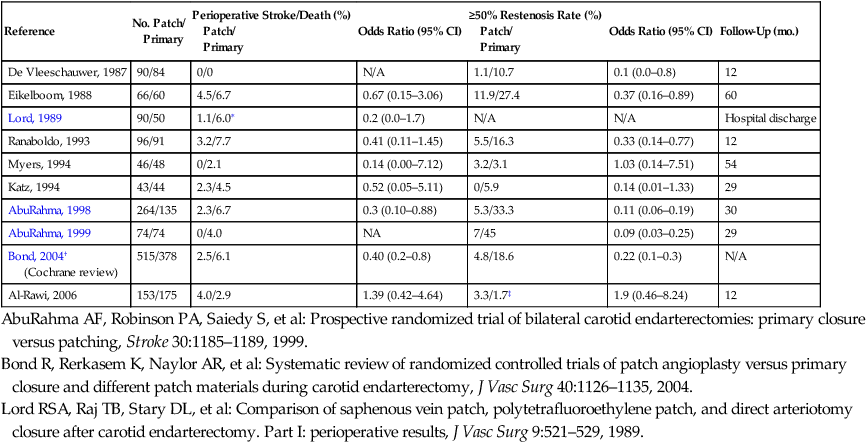
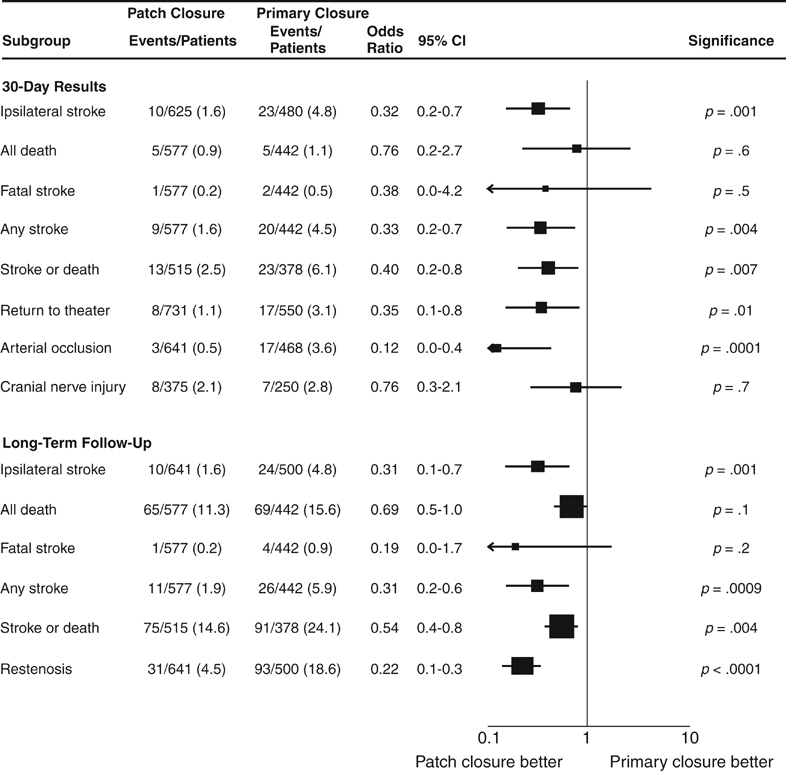
Several randomized, controlled trials (Level I evidence) have been published since the 1990s comparing CEA with patch angioplasty versus primary closure. Table 1 summarizes the results of these randomized, controlled trials. As noted in this table, these trials showed the superiority of patch closure over primary closure in reducing the perioperative stroke or death and the incidence of significant restenosis. TABLE 1 Results of Randomized, Controlled Trials of Carotid Endarterectomy with Patch Closure versus Primary Closure CI, Confidence interval; N/A, not available or not applicable. ∗Includes 30-day risk of ipsilateral stroke only. †This is a meta-analysis of several randomized trials. ‡Carotid occlusion only (not ≥50% restenosis). AbuRahma AF, Robinson PA, Saiedy S, et al: Prospective randomized trial of carotid endarterectomy with primary closure and patch angioplasty with saphenous vein, jugular vein, and polytetrafluoroethylene: long-term follow-up, J Vasc Surg 27:222–234, 1998. AbuRahma AF, Robinson PA, Saiedy S, et al: Prospective randomized trial of bilateral carotid endarterectomies: primary closure versus patching, Stroke 30:1185–1189, 1999. Bond R, Rerkasem K, Naylor AR, et al: Systematic review of randomized controlled trials of patch angioplasty versus primary closure and different patch materials during carotid endarterectomy, J Vasc Surg 40:1126–1135, 2004. Lord RSA, Raj TB, Stary DL, et al: Comparison of saphenous vein patch, polytetrafluoroethylene patch, and direct arteriotomy closure after carotid endarterectomy. Part I: perioperative results, J Vasc Surg 9:521–529, 1989. In addition, there were two meta-analyses of the randomized, controlled carotid trials by the Cochrane Collaboration in 2000 and 2004. In an earlier Cochrane meta-analysis of randomized carotid trials, the early postoperative thrombosis, postoperative stroke, and at least 50% restenosis were superior for patching, in contrast to primary closure. In an update of the Cochrane Collaboration meta-analysis in 2004, Bond and colleagues reported the outcome for 1281 patients, including seven controlled carotid trials. Patch angioplasty was associated with a reduction in ipsilateral stroke (1.6% versus 4.8% for primary closure, p = .001), any stroke (1.6% vs. 4.5%, p = .004), stroke or death (2.5% vs. 6.1%, p = .007), arterial occlusion (0.5% vs. 3.6%, p = .0001), and return to the operating room (1.1% vs. 3.1%, p = .01). In long-term follow-up, patch angioplasty was also superior to primary closure in the reduction of ipsilateral stroke (1.6% vs. 4.8%, p = .001), any stroke (1.9% vs. 5.9%, p = .0009), stroke or death (14.6% vs. 24%, p = .004), and late restenosis (4.8% vs. 18.6%, p < .0001) (Figure 1).
Patch Graft Closure with Carotid Endarterectomy
Patch Closure Versus Primary Closure
Reference
No. Patch/
Primary
Perioperative Stroke/Death (%)
Patch/
Primary
Odds Ratio (95% CI)
≥50% Restenosis Rate (%)
Patch/
Primary
Odds Ratio (95% CI)
Follow-Up (mo.)
De Vleeschauwer, 1987
90/84
0/0
N/A
1.1/10.7
0.1 (0.0–0.8)
12
Eikelboom, 1988
66/60
4.5/6.7
0.67 (0.15–3.06)
11.9/27.4
0.37 (0.16–0.89)
60
Lord, 1989
90/50
1.1/6.0∗
0.2 (0.0–1.7)
N/A
N/A
Hospital discharge
Ranaboldo, 1993
96/91
3.2/7.7
0.41 (0.11–1.45)
5.5/16.3
0.33 (0.14–0.77)
12
Myers, 1994
46/48
0/2.1
0.14 (0.00–7.12)
3.2/3.1
1.03 (0.14–7.51)
54
Katz, 1994
43/44
2.3/4.5
0.52 (0.05–5.11)
0/5.9
0.14 (0.01–1.33)
29
AbuRahma, 1998
264/135
2.3/6.7
0.3 (0.10–0.88)
5.3/33.3
0.11 (0.06–0.19)
30
AbuRahma, 1999
74/74
0/4.0
NA
7/45
0.09 (0.03–0.25)
29
Bond, 2004†
(Cochrane review)
515/378
2.5/6.1
0.40 (0.2–0.8)
4.8/18.6
0.22 (0.1–0.3)
N/A
Al-Rawi, 2006
153/175
4.0/2.9
1.39 (0.42–4.64)
3.3/1.7‡
1.9 (0.46–8.24)
12
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
