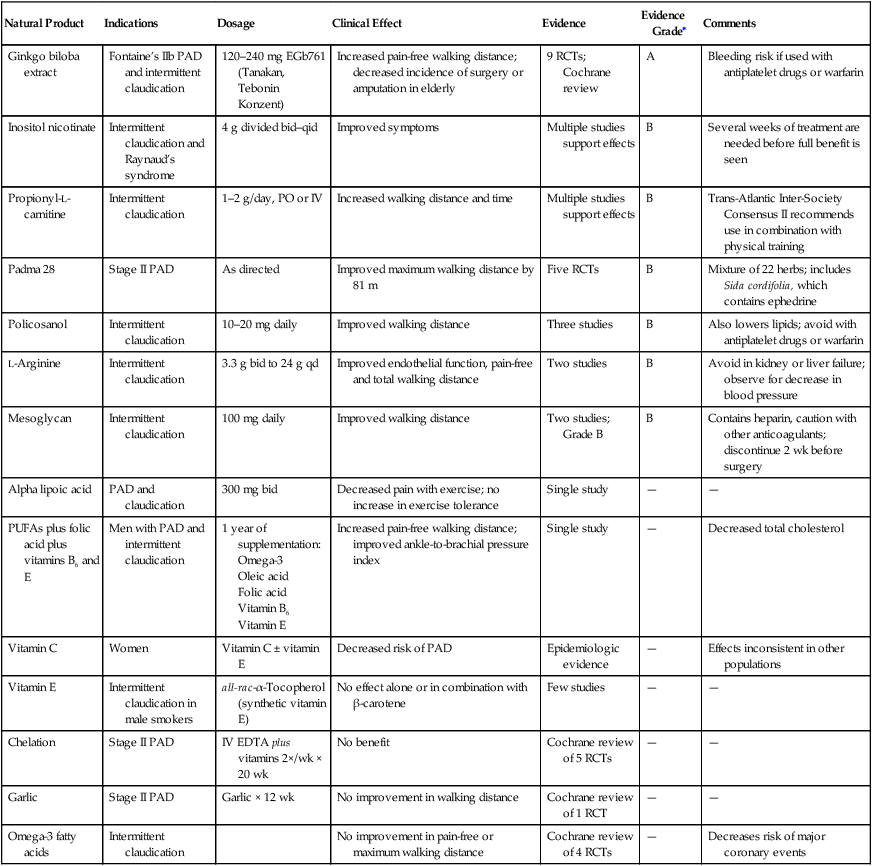
Natural products for peripheral arterial disease are listed in Table 1. TABLE 1 Natural Products for Peripheral Arterial Disease ∗Evidence grades: A, statistically significant evidence of benefit from randomized trials and/or meta-analysis; B, statistically significant evidence of benefit from randomized trials or nonrandomized studies.
Integrative Therapies in Vascular Disease
Natural Products for Peripheral Arterial Disease
Natural Product
Indications
Dosage
Clinical Effect
Evidence
Evidence Grade∗
Comments
Ginkgo biloba extract
Fontaine’s IIb PAD and intermittent claudication
120–240 mg EGb761 (Tanakan, Tebonin Konzent)
Increased pain-free walking distance; decreased incidence of surgery or amputation in elderly
9 RCTs; Cochrane review
A
Bleeding risk if used with antiplatelet drugs or warfarin
Inositol nicotinate
Intermittent claudication and Raynaud’s syndrome
4 g divided bid–qid
Improved symptoms
Multiple studies support effects
B
Several weeks of treatment are needed before full benefit is seen
Propionyl-L-carnitine
Intermittent claudication
1–2 g/day, PO or IV
Increased walking distance and time
Multiple studies support effects
B
Trans-Atlantic Inter-Society Consensus II recommends use in combination with physical training
Padma 28
Stage II PAD
As directed
Improved maximum walking distance by 81 m
Five RCTs
B
Mixture of 22 herbs; includes Sida cordifolia, which contains ephedrine
Policosanol
Intermittent claudication
10–20 mg daily
Improved walking distance
Three studies
B
Also lowers lipids; avoid with antiplatelet drugs or warfarin
L-Arginine
Intermittent claudication
3.3 g bid to 24 g qd
Improved endothelial function, pain-free and total walking distance
Two studies
B
Avoid in kidney or liver failure; observe for decrease in blood pressure
Mesoglycan
Intermittent claudication
100 mg daily
Improved walking distance
Two studies; Grade B
B
Contains heparin, caution with other anticoagulants; discontinue 2 wk before surgery
Alpha lipoic acid
PAD and claudication
300 mg bid
Decreased pain with exercise; no increase in exercise tolerance
Single study
—
—
PUFAs plus folic acid plus vitamins B6 and E
Men with PAD and intermittent claudication
1 year of supplementation:
Omega-3
Oleic acid
Folic acid
Vitamin B6
Vitamin E
Increased pain-free walking distance; improved ankle-to-brachial pressure index
Single study
—
Decreased total cholesterol
Vitamin C
Women
Vitamin C ± vitamin E
Decreased risk of PAD
Epidemiologic evidence
—
Effects inconsistent in other populations
Vitamin E
Intermittent claudication in male smokers
all-rac-α-Tocopherol (synthetic vitamin E)
No effect alone or in combination with β-carotene
Few studies
—
—
Chelation
Stage II PAD
IV EDTA plus vitamins 2×/wk × 20 wk
No benefit
Cochrane review of 5 RCTs
—
—
Garlic
Stage II PAD
Garlic × 12 wk
No improvement in walking distance
Cochrane review of 1 RCT
—
—
Omega-3 fatty acids
Intermittent claudication
No improvement in pain-free or maximum walking distance
Cochrane review of 4 RCTs
—
Decreases risk of major coronary events
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
