Paroxysmal Supraventricular Tachycardia
Hakan Oral
Fred Morady
Supraventricular tachycardias arise in or involve at least some part of the atrium or atrioventricular junction. Supraventricular tachycardias develop as a result of abnormal automaticity, triggered activity, or most commonly, reentry. Both atrial flutter and atrial fibrillation are supraventricular tachycardias; however, because of the differences in their mechanisms and clinical manifestations, they are grouped separately from other types of supraventricular tachycardias, commonly referred to as paroxysmal supraventricular tachycardia (PSVT).
USUAL CAUSES AND MECHANISMS OF SUPRAVENTRICULAR TACHYCARDIA
The most common forms of PSVT are atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reciprocating tachycardia (AVRT), and atrial tachycardia. Together these constitute more than 95% of all PSVTs. Uncommon mechanisms of PSVT include sinus node reentry, junctional ectopic tachycardia, intra-Hisian reentry, and nodoventricular or nodofascicular reentrant tachycardias (Table 16.1). In addition, the symptoms of PSVT sometimes are mimicked by sinus tachycardia.
Atrioventricular Nodal Reentrant Tachycardia
AVNRT is the most common type of PSVT encountered in clinical practice, accounting for approximately two thirds of all cases. AVNRT is more commonly seen in women, with a female-to-male gender ratio of 2:1. It may occur at any age but most commonly manifests during the fourth and fifth decades of life.
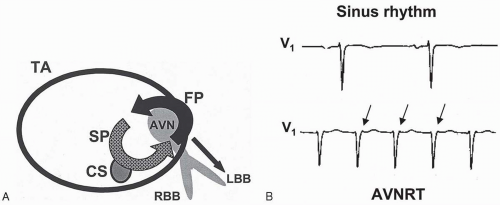
AVNRT is caused by reentry. In patients with AVNRT, the atrioventricular junction has two or more functionally discrete pathways. One of these functional pathways, the “fast pathway,” conducts impulses rapidly but has a relatively long effective refractory period. The other pathway, “slow pathway,” has a slower conduction velocity but a shorter effective refractory period than the fast pathway (1,2). In typical AVNRT, an atrial premature depolarization (APD) conducts to the atrioventricular junction through the atrium. Because it is premature, it may encounter a refractory fast pathway and conduct through only the slow pathway. Because the slow pathway has a longer conduction time, by the time the depolarization travels through the slow pathway and arrives at the compact atrioventricular junction, the fast pathway may have recovered excitability, so that the depolarization travels in a retrograde manner through the fast pathway and back down the slow pathway. If this reentry process continues, a sustained tachycardia occurs (Fig. 16.1) (3,4,5). Because the fast pathway has a rapid conduction velocity, the ventriculoatrial conduction time during typical AVNRT is very short. Therefore on the surface electrocardiogram (ECG), retrograde P waves may be buried within the QRS complexes
and not be visible or may be partially visible at the end of the QRS complex (Fig. 16.1). P waves are typically inverted in the inferior leads (II, III, and aVF) and may be manifest as pseudo-S waves, and upright in V1, leading to a pseudo-r′ appearance.
and not be visible or may be partially visible at the end of the QRS complex (Fig. 16.1). P waves are typically inverted in the inferior leads (II, III, and aVF) and may be manifest as pseudo-S waves, and upright in V1, leading to a pseudo-r′ appearance.
TABLE 16.1. Paroxysmal supraventricular tachycardias | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In the atypical form of AVNRT, the fast pathway is used as the anterograde limb, and the slow pathway, as the retrograde limb of the reentrant circuit. Therefore the ventriculoatrial conduction time is prolonged. The ECG reveals inverted P waves in the inferior leads and a long RP interval (RP interval exceeds PR interval). Atypical AVNRT accounts for fewer than 10% of cases of AVNRT.
Atrioventricular Reentrant Tachycardia (AVRT)
In normal individuals, the only electrical connections between the atria and the ventricles are the atrioventricular node and the His-Purkinje system. In patients who have an accessory pathway, an extra muscular tissue exists between the atrium and the ventricle. Accessory pathways may conduct electrical impulses in an anterograde or retrograde manner or in both directions. Accessory pathways that conduct only in the retrograde direction are called concealed accessory pathways, because no delta waves are present on the ECG. Anterograde conduction over an accessory pathway leads to ventricular preexcitation, with the typical ECG manifestations of a short PR interval and delta waves (Wolf-Parkinson-White pattern). Depending on the relative timing of the activation of the ventricles through the atrioventricular junction, the His bundle,
and the accessory pathway, different degrees of ventricular preexcitation may be present, and the delta waves may be subtle or pronounced.
and the accessory pathway, different degrees of ventricular preexcitation may be present, and the delta waves may be subtle or pronounced.
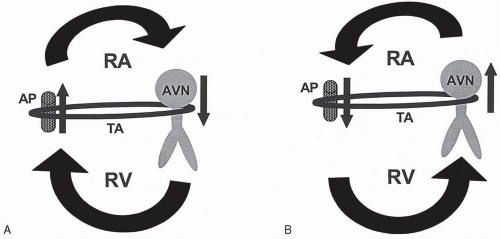
The mechanism of PSVT due to an accessory pathway is reentry. An APD may block the accessory pathway in an anterograde manner and then activate the ventricle through the atrioventricular node and the His bundle. By the time the impulse reaches the ventricular insertion site of the accessory pathway, the pathway may have regained excitability and may conduct in a retrograde manner, initiating the tachycardia. This type of reentry, in which the atrioventricular node and the His bundle are used as the anterograde limb, and the accessory pathway, as the retrograde limb, is called orthodromic reciprocating tachycardia (ORT) (Figs. 16.2A and 16.3). Approximately 30% of PSVTs arise from orthodromic reciprocating tachycardia (Table 16.1). The type of reentry circuit in which the accessory pathway is used as the anterograde limb and the atrioventricular node-His-Purkinje system is used as the retrograde limb is referred to as antidromic reciprocating tachycardia (ART) (Figs. 16.2B and 16.4).
The anatomic location of the accessory pathway may be anteroseptal, midseptal, posteroseptal, right free wall, or left free wall. Free-wall sites are subgrouped as anterior, anterolateral, lateral, posterolateral, or posterior in relation to the mitral or tricuspid annulus. Left free-wall pathways account for 60% of all pathways, followed by posteroseptal (30%) and right free-wall pathways (10%). The anteroseptal and midseptal pathways are rare. Multiple accessory pathways exist in 5% of patients with the Wolff-Parkinson-White syndrome. Multiple accessory pathways are more prevalent among patients with congenital heart disease, particularly the Ebstein anomaly.
The most common type of supraventricular tachycardia in patients with an accessory pathway is ORT. ART accounts for fewer than 10% of accessory pathway-mediated PSVTs.
An unusual PSVT is the permanent form of junctional reciprocating tachycardia, an
ORT in which a slowly conducting, concealed posteroseptal pathway is used as the retrograde limb of the reentrant circuit. This tachycardia has a long RP interval, with inverted P waves in the inferior leads. It may be incessant and may cause tachycardia-induced cardiomyopathy (Fig. 16.5).
ORT in which a slowly conducting, concealed posteroseptal pathway is used as the retrograde limb of the reentrant circuit. This tachycardia has a long RP interval, with inverted P waves in the inferior leads. It may be incessant and may cause tachycardia-induced cardiomyopathy (Fig. 16.5).
Atrial Tachycardia
Atrial tachycardias account for approximately 10% of all PSVT. In contrast to AVNRT and AVRT, which are caused by reentry, the mechanism of atrial tachycardia may be abnormal automaticity, triggered activity, or reentry, particularly in patients with scarred atrial myocardium. Atrial tachycardia may originate in the right atrium, typically along the crista terminalis, or in the left atrium. In patients with atrial tachycardia, variable atrioventricular conduction may be present, and atrial tachycardia persists even with atrioventricular block. In contrast, ORT and ART cannot continue with atrioventricular block.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree