Parathyroid Adenoma
Presentation
A 31-year-old man with a history of renal failure, joint pain, weakness, and persistently elevated serum calcium recently underwent a 3.5-gland parathyroidectomy followed by a neck reexploration and retrieval of the remaining para-thyroid for persistent hypercalcemia.
Differential Diagnosis
Ninety percent of patients with hypercalcemia have either primary hyperparathy-roidism or malignancy. Primary hyperparathyroidism may be due to solitary adenomas or multiple endocrine neoplasia. In the case of malignancy, hypercalcemia is a serum abnormality found during the clinical evaluation for the patient’s symptoms associated with the malignancy. These symptoms may include weight loss, fatigue, and night sweats. Malignancies that may cause hypercalcemia include metastatic breast cancer and solid tumors such as lung and renal cancers. Additionally, hematologic malignancies, such as lymphoma, leukemia, and multiple myeloma, may also cause hypercalcemia.
Less common causes for hypercalcemia include vitamin D intoxication, idiopathic hypercalcemia of infancy, hyperthyroidism, thiazide diuretics, and vitamin A intoxication. When associated with renal failure, etiologies for hypercalcemia include severe secondary hyperparathyroidism, aluminum intoxication, and milk-alkali syndrome.
Discussion
In this scenario, the patient undergoes two neck dissections and removal of all four parathyroid glands, which on histologic examination demonstrates parathyroid hyperplasia. Despite the removal of all parathyroid tissue in the neck, hypercalcemia (9.5 to 12.0 mg/dL) and severely elevated parathyroid hormone levels (1,200 to 1,700 mg/dL) persist.
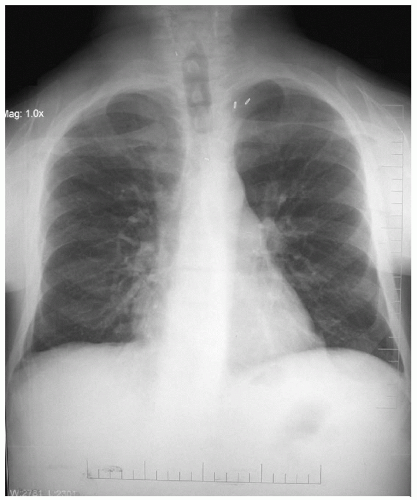
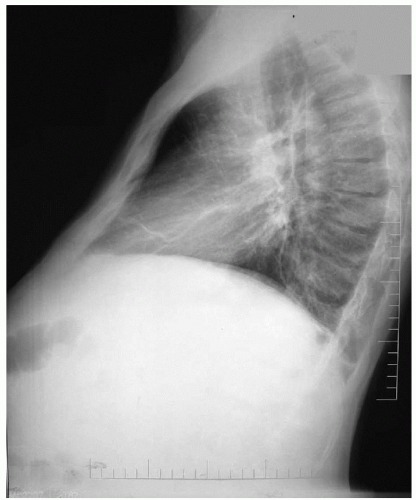
Although all parathyroid tissue is removed from the neck, ectopic para thyroid tissue can still be present. Embryonically, the superior and inferior parathyroid glands develop separately. The superior para thyroid glands arise from the fourth branchial pouch along the posterolateral lobes of the thyroid gland. The inferior para thyroid glands develop from the third branchial pouch and migrate with the thymus; ectopic parathyroid may be found in the anterior mediastinum and, less commonly, in the middle and posterior mediastinum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree