Paraseptal and Interstitial Emphysema
Marie-Christine Aubry, M.D.
Allen P. Burke, M.D.
Paraseptal Emphysema
Definition
Paraseptal (distal acinar) emphysema is the third major subtype of emphysema, after centrilobular (Chapter 44) and panlobular emphysema (Chapter 45). It differs from centrilobular and panlobular emphysema by involving the distal portion of the acinus. Although the pathogenesis of centrilobular and panlobular emphysema is attributed to the imbalance between proteases and antiproteases leading to the destruction of the alveolated lung parenchyma, the pathogenesis of paraseptal emphysema is less certain.1
Clinical Findings
Paraseptal emphysema is associated with the formation of apical bullae, a bulla being defined as an enlarged airspace of >1 cm. In isolation, it is seen predominantly in men presenting with a spontaneous pneumothorax and otherwise no increase in symptoms and no airflow limitation.
Most often, paraseptal emphysema is seen in association with centrilobular emphysema in smokers. A small subset (<10%) of smokers with emphysema will have predominantly paraseptal emphysema on computed tomography scans.2
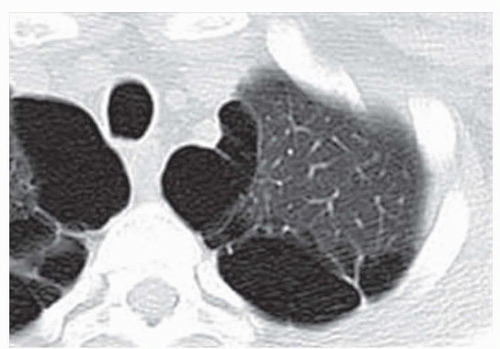
Radiologic Findings
Gross Findings
The gross findings mimic the radiologic findings. Paraseptal emphysema is usually subpleural, more frequent in the upper lobes (Fig. 46.2). Bullae are typically present in resected specimens. The dilated airspaces are often collapsed and may not be nearly as dramatic as the appearance by computed tomographic scans.
Microscopic Findings
In paraseptal emphysema, the alveolar ducts are enlarged with destruction of distal alveolar septa. Bulla appears often as thin-walled cysts with fibrous wall. The adjacent lung parenchyma appears normal unless there is associated centrilobular emphysema.
Prognosis and Treatment
When in isolation, paraseptal emphysema is not associated with any physiologic abnormality. The main complication is formation of bulla, which may lead to recurrent spontaneous pneumothorax. Treatment includes tube thoracotomy and surgical resection of abnormal lung.3
Pulmonary Interstitial Emphysema
Definition
In contrast to the major types of emphysema, pulmonary interstitial emphysema (PIE) is a fundamentally different process in that the formation of the enlarged airspaces is not related to destruction of alveolar septa. In contrast, interstitial emphysema is the result of air dissecting through the alveolar walls into the adjacent interstitial tissues where it forms cystic spaces.
Clinical Findings
PIE is seen primarily in four settings: in neonates with premature lung disease on mechanical ventilation, in adults with centrilobular emphysema, in adults with underlying fibrotic lung disease, and in adults on mechanical ventilation. The major risk factors for the development of PIE in infants are very low birth weight and mechanical ventilation for respiratory distress syndrome. PIE may rarely occur in infants on continuous positive airway pressure (CPAP) who are not mechanically ventilated.4 Occasional reports describe infants developing PIE in the setting of laryngeal disease or pneumonia in the absence of mechanical ventilation or CPAP.4 PIE in infants is often associated with pneumothorax or pneumomediastinum.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree