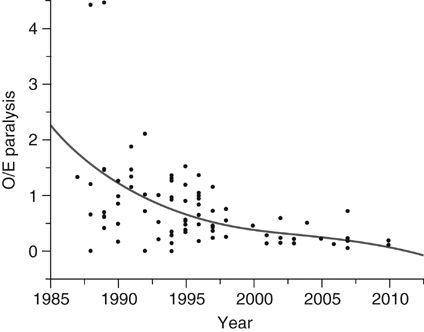
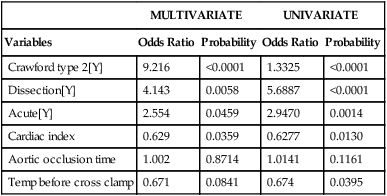
The overlapping effects of aortic occlusion, collateral blood flow, metabolism, oxygen supply and demand, surgical technique, and response to ischemia underlie the unpredictability of spinal cord ischemia and subsequent paralysis in the surgical treatment of thoracoabdominal aortic aneurysms (TAAAs). However, experimentally validated interventions that enhance collateral circulation, increase ischemic tolerance, and add neurochemical protection have reduced the paraplegia risk by 80% to 90% since the 1980s (Figure 1). These factors have been assessed before, during, and after aortic occlusion, and multivariate modeling has been used to stratify them based on statistical significance to quantify their relative importance in reducing paralysis when acting simultaneously (Table 1). Extent of aortic replacement, acuity, and cardiac function are more important than temperature and occlusion time, which suggests that deleterious changes in other critical factors, such as CSF pressure, cardiac function, and oxygen delivery after aortic occlusion, are the underlying problem with longer aortic occlusion times. TABLE 1 Clinical and Physiologic Factors Most Important as Determinants for Risk of Paralysis∗ ∗Extent of aortic replacement (Crawford type 2), acute presentation (rupture and dissection), and change in cardiac index with aortic occlusion are more important than aortic occlusion time and moderate hypothermia, which were significant univariate factors. For each unit increase in cardiac index the paralysis risk declined, as it did for each unit decrease in temperature. Strategies to reduce spinal cord ischemia have fallen into four areas of clinical investigation and intervention: direct anatomic perfusion and reconstruction of spinal cord circulation, manipulation of cord metabolism with drugs and hypothermia to prolong ischemic tolerance and reduce reperfusion injury, augmenting collateral blood flow by controlling hemodynamics, controlling CSF pressure, and combinations of these therapies. To compare clinical reports of paralysis outcomes for thoracoabdominal aortic replacement, we developed an accurate mathematical model of paralysis risk, which accounted for 97% of the variability in paralysis rates in clinical reports up to that time (Table 2). This model confirmed, as do most clinical reports, that paralysis risk is a function of the amount of aorta replaced and clinical presentation and that paralysis risk is also technique dependent. The ratio of observed to expected number of deficits (O/E ratio) is a quantitative measure of the effectiveness of different spinal cord protective strategies. The model makes it possible to compare different techniques such as simple aortic occlusion with intercostal reimplantation with and without assisted circulation, which have O/E ratios of 1 (1.15 and 0.98) (see Table 2). TABLE 2 Actual and Predicted Paraplegia Risk by Repair Technique
Paraplegia Prevention in Thoracic and Thoracoabdominal Aortic Aneurysm Repair
MULTIVARIATE
UNIVARIATE
Variables
Odds Ratio
Probability
Odds Ratio
Probability
Crawford type 2[Y]
9.216
<0.0001
1.3325
<0.0001
Dissection[Y]
4.143
0.0058
5.6887
<0.0001
Acute[Y]
2.554
0.0459
2.9470
0.0014
Cardiac index
0.629
0.0359
0.6277
0.0130
Aortic occlusion time
1.002
0.8714
1.0141
0.1161
Temp before cross clamp
0.671
0.0841
0.674
0.0395
Technique
Total Patients
Paralysis O/E Ratio
AC
1289
1.13
AC+SFD
434
0.44
AC+SFD+
6133
0.28
XCL
4244
0.98
XCL+SFD
619
0.50
XCL+SFDN
1581
0.18
XCL+SFDN+IC
385
0.11
HCA
322
0.43
HCA+SFD
526
0.15
TEVAR
531
1.04
TEVAR+S FD
456
0.56
Totals
16,138
0.53 ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine
