Paradoxical Embolism
BENJAMIN JACOBS, ANDREW KIMBALL, and THOMAS W. WAKEFIELD
Presentation
A 59-year-old woman presents to an outside institution with right-sided facial droop, right-sided hemiplegia, mild aphasia, and hypoxemia. She is resuscitated and put on oxygen with resolution of her hypoxemia. A computed tomography (CT) scan of the head was unremarkable, and a spiral chest CT scan revealed bilateral pulmonary emboli (PE). At this point, the patient is stabilized and transferred to your hospital.
On admission, the patient reports acute-onset shortness of breath and right-sided weakness roughly 12 hours ago. Without prompting, the patient recalls that 4 weeks ago she fell and dislocated her patella. She saw an orthopedic surgeon at that time––who recommended bed rest and non–weight bearing on that extremity. She continues to complain of pain in her left lower extremity. On exam, the patient is afebrile and in no respiratory distress. Vital signs reveal a regular pulse of 95 beats per minute, respiratory rate 22, and blood pressure 134/79; pulse oximetry is 91% on 4 L of oxygen and 100% on 100% oxygen by face mask. On physical examination, a systolic ejection murmur is appreciated; lungs are clear; there is ecchymosis of the left patella extending down to the shin without erythema or tenderness. Neurologic examination is significant for right-sided hemianopsia, facial droop, aphasia, and upper and lower extremity weakness.
Differential Diagnosis
The differential diagnosis in this case includes
1. Cerebral vascular accident (CVA––cardioembolic or thromboembolic)
2. Deep venous thrombosis with pulmonary embolism (DVT/PE)
3. CVA and DVT/PE
4. Paradoxical embolism––simultaneous DVT/PE and CVA from a venous embolus traversing a right-to-left shunt into the arterial system.
Initial Workup
In this case, a paradoxical embolism would account for all of the patient’s symptoms and does not make the assumption that two conditions are happening simultaneously. Given concern for a paradoxical embolism, a transthoracic echocardiogram (TTE) with agitated saline injection (“bubble test”) is ordered to look for a patent foramen ovale (PFO), and a lower extremity duplex scan is ordered to look for a DVT. Of note, transesophageal echocardiography (TEE) is considered more sensitive for the detection of a PFO––and should be ordered if the TTE is nondiagnostic.
Lower Extremity Duplex Scan
The lower extremity duplex scan reveals evidence of an acute DVT of the left leg involving the posterior tibial, peroneal, and anterior tibial veins.
Transthoracic Echocardiography with “Bubble Test”
The TTE with bubble test reveals no evidence of PFO––although the exam is limited by the patient’s body habitus.
Transesophageal Echocardiography with “Bubble Test”
The TEE with bubble test reveals clear evidence of a PFO with right to left shunt. Of note, there is no valvular vegetations or intra-atrial thrombus.
Case Continued
The diagnosis of paradoxical embolism is made based on the clinical history and clear objective evidence of DVT/PE, a right-to-left shunt, and arterial embolism. The day after admission, a noncontrast head CT demonstrates mass effect consistent with a left cerebral nonhemorrhagic infarct. Given concern for hemorrhagic conversion of her stroke, she is not anticoagulated immediately and a Greenfield filter is placed. Three days after admission, the patient complains of increased right-sided weakness. She undergoes carotid duplex imaging.
Carotid Duplex Scan
Duplex Scan Report
A heterogeneous embolus (arrow) in the left common carotid artery creating a 60% to 80% diameter stenosis with instability is found (Fig. 1). The distal end of the embolus is imaged.
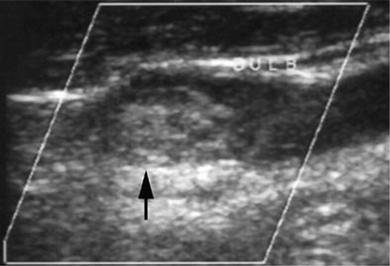
FIGURE 1 Echogenic embolus (arrow) just below left carotid bulb. (Reproduced from Gada H, Jafer M, Graziano K, et al. Carotid embolectomy in the treatment of a paradoxical embolus. Ann Vasc Surg. 2003;17:457–461, with permission.)
Surgical Approach
The diagnosis of paradoxical embolus (PDE) to the left carotid artery is made. The patient is taken to the operating room for embolectomy, because the embolus appears to be unstable with the potential to cause further cerebrovascular injury. After systemic heparin administration, the left carotid artery is opened, revealing a large embolus at the carotid bifurcation. This embolus is removed, but because adequate retrograde flow is not obtained, a 3-French Fogarty catheter is carefully passed, extracting a tail of thrombus (6 cm long; Fig. 2). A number 12 shunt is rapidly placed, and flow is documented using Doppler. The arteriotomy is closed with a patch, and minimal atherosclerotic disease is found. A completion intraoperative duplex scan reveals excellent flow through the carotid and no debris (Fig. 3). The patient is awakened on the table and taken to the recovery room, where she remains stable. Her neurologic examination remains unchanged.

FIGURE 2 Operative specimen revealing embolus. Arrow demonstrates echogenic embolus and correlates to the preoperative duplex image (see Fig. 55-1A). Double arrows point to thrombus tail. (Reproduced from Gada H, Jafer M, Graziano K, et al. Carotid embolectomy in the treatment of a paradoxical embolus. Ann Vasc Surg. 2003;17:457–461, with permission.)
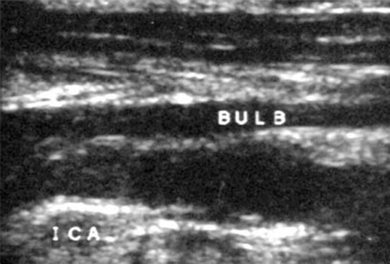
FIGURE 3 Postprocedure duplex scan reveals no abnormalities. (Reproduced from Gada H, Jafer M, Graziano K, et al. Carotid embolectomy in the treatment of a paradoxical embolus. Ann Vasc Surg. 2003;17(4):457–461, with permission.)



