Pacemaker and ICD Insertions
Mani Arsalan
J. Michael DiMaio
James R. Edgerton
Introduction
Since the first pacemaker implantation in 1958 by Elmquist and Senning, these devices have become highly engineered, reliable, and durable. While the first generation of pacemakers could only pace the heart at a specific rate, modern devices can be adapted to patient needs by mimicking the native conduction system. The introduction of transvenous lead implantation reduced the invasiveness of the procedure, and currently leadless pacemakers are available for implantation. The development of noninvasive programming of pacemakers has been another great improvement from the first generation. Further, new devices record and store electrocardiograms and some models even permit telemonitoring. Today, permanent pacemaker implantation (PPM) is a routine and safe procedure performed by cardiac surgeons and cardiologists. That more than 700,000 new PPM are implanted annually highlights the importance of this treatment. Temporary pacemakers are used to bridge short-term arrhythmias (e.g., caused by myocardial infraction), in case of emergencies and after cardiac surgery. For chronic cardiac rhythm dysfunction PPM is indicated. In the first portion of this chapter we focus on PPM.
Sinus Node Dysfunction
Pacemaker implantation is the only effective therapy for chronic symptomatic sinus node dysfunction (SND). The risk for sudden death in patients with SND is very low, so relief of symptoms of SND is the major goal in PPM implantation because implantation does not appear to prolong survival. SND (bradycardia, sinus pause, and chronotropic incompetence) is a Class Ic indication for PPM implantation according to the American College of Cardiology/American Heart Association
(ACC/AHA) guidelines. Iatrogenic bradycardia caused by required drug therapy for various medical conditions is another indication. PPM implantation is also reasonable for syncope of unexplained origin when abnormalities of the sinus node are discovered during work-up. The need for PPM, in this case, is determined by the frequency and duration of sinus pauses and the patient’s symptomatic response to them.
(ACC/AHA) guidelines. Iatrogenic bradycardia caused by required drug therapy for various medical conditions is another indication. PPM implantation is also reasonable for syncope of unexplained origin when abnormalities of the sinus node are discovered during work-up. The need for PPM, in this case, is determined by the frequency and duration of sinus pauses and the patient’s symptomatic response to them.
Atrioventricular Block
Decision making regarding PPM implantation due to atrioventricular (AV) block is based on its degree, permanence, and etiology.
In first-degree block, the PR interval is prolonged beyond 200 ms, but this prolongation is not associated with any symptoms and, thus, has no direct clinical consequences.
In second-degree AV block, a dissociation of the atria and ventricles exists. This is usually asymptomatic, with rare cases of presyncope or syncope. Bradycardia on physical examination and palpitations may occur. A distinction is made between Mobitz I (Wenckebach) with progressive PR interval prolongation followed by an eventual drop in QRS complex and Mobitz II that has dropped beats without prior PR prolongation. Mobitz II is often described by its ratio of nonconducted P waves to conducted QRS complex (e.g., two P waves for every one QRS complex is described as 2:1 Mobitz II block). While Mobitz I is almost always a benign AV node disease, Mobitz II is caused by pathology in the His–Purkinje system and more often progresses into complete AV block.
Third-degree AV block (complete AV block) is a complete dissociation between the atria and ventricles. As accessory pacemakers in the lower chambers typically activate the ventricles, the atrial rate exceeds the ventricular rate. The resulting bradycardia may lead to fatigue, dizziness, presyncope, and syncope.
AV block has a variety of possible etiologies. Several drugs can block AV conduction (e.g., beta-blockers, digitalis, and calcium channel blockers). Other reasons include infective endocarditis, Lyme disease, sarcoidosis, and acute myocardial ischemia or infarction. Procedures such as alcohol septal ablation in patients with obstructive hypertrophic cardiomyopathy or heart valve surgery (especially transcatheter aortic valve replacement) are also associated with the development of AV block.
Reversible causes of AV block, like nonessential medications or electrolyte abnormalities, should be fixed prior to considering PPM implantation. Unless persistent symptoms are present, first-degree and Mobitz I AV block do not require PPM implantation. Mobitz II, especially with a wide QRS, may progress into complete AV block and thus should be considered for PPM implantation. ACC/AHA guidelines state that symptomatic Mobitz II and third-degree AV block should be treated by PPM implantation unless the AV block is expected to resolve and is unlikely to recur. Asymptomatic patients with Mobitz II or third-degree block may be considered for PPM implantation.
Cardiac Resynchronization Therapy
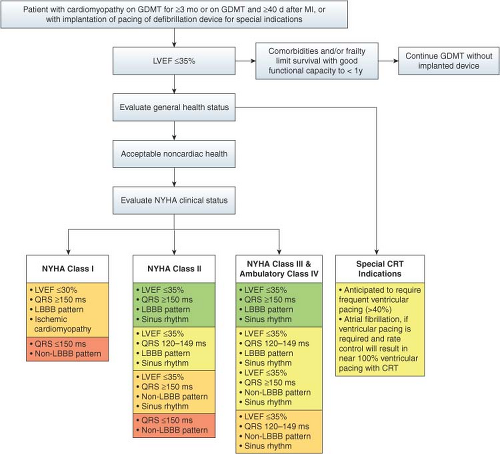
Cardiac resynchronization therapy (CRT) is primarily indicated in patients with cardiomyopathy associated with a wide QRS complex. CRT is intended to improve left ventricular (LV) function by reestablishing the synchrony of the left ventricle. Several studies have shown that PPM implantation reduces symptoms, hospitalization, and mortality compared with conventional therapy. The 2012 updated AHA/AVV guidelines for PPM implantation in CRT include patients with NYHA Class II or higher and a left bundle branch block with a QRS duration greater than or equal to 150 ms. An algorithm for CRT indications is presented in Figure 39.1.
Technology
Pacemaker Generator
The decrease in size and increase in complexity of integrated chip technology has led to smaller, more reliable cardiac implantable electrical devices (CIED), which can be interrogated. Modern CIEDs consist of a lithium iodide battery, integrated circuits, and a telemetry antenna. While some devices can only be interrogated with a manufacturer-specific programmer via contact between the programmer wand and the skin above the device, newer pacemakers have wireless capabilities that allow for remote patient follow-up and monitoring.
Leads
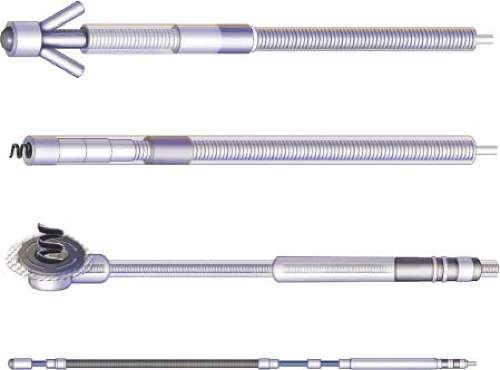
Pacemaker leads are composed of a connector pin, conductor, insulation, electrode, and fixation device (Fig. 39.2). They can be distinguished as epicardial or endocardial leads. Endocardial leads are most commonly employed. Endocardial leads are fixed in the myocardium by passive fixation with barbs (captured in the trabeculae) or active fixation with screws. Active fixation can be facilitated by either fixed or retractable screws and provides secure fixation in locations with low trabeculation or the atrium. Epicardial leads are used in special situations or as a bail-out when endocardial leads insertion is not possible (e.g., mechanical tricuspid valve, endocarditis, infected CIED, or venous access problems), in congenital heart disease, or during cardiac surgery when postoperative PPM implantation is required. Specialized techniques for these situations will be described.
In the past, the implantation of a single-chamber (atrial-only lead) PPM was the treatment of choice in sinus node disease. But, several studies have demonstrated that many patients with sinus node dysfunction need an upgrade to a dual-chamber PPM due to development of AV block with atrial fibrillation and bradycardia. A Danish multicenter randomized trial showed a higher rate of major complications after system upgrades, while the risk after first implantation of single- and dual-chamber PPM were similar. Thus in the vast majority of cases, dual-chamber PPM are now implanted initially. However, a single-chamber PPM may be indicated in isolated sinus node disease when any AV conduction disease, including type I AV block, is excluded. Similarly, as isolated ventricular pacing may lead to a 15% to 30% reduction in cardiac output, pacemaker syndrome, and atrial fibrillation, isolated ventricular pacing is only indicated in chronic atrial fibrillation or when patients will have a low frequency of active pacing (e.g., demand pacemaker due to carotid sinus syndrome). Table 39.1 summarizes the indications for single- and dual-chamber PPM.
Pacemaker Code and Programming
Pacemaker function is described using a five-letter standard NBG code developed by the North American Society of Pacing and Electrophysiology (NASPE) and British Pacing and Electrophysiology Group (BPEG). Most commonly, the first three letters are
used. The first three letters specify the chamber(s) paced, the chamber(s) sensed, and the pacing algorithm (response to a sensed beat), respectively. The NBG code is summarized in Table 39.2. The choice of the specific pacemaker and its programming is adjusted to fit the patient needs. For example, in sick sinus syndrome, a dual-chamber PPM could be implanted with a DDD-backup mode programmed. Thus, the PPM would pace AAI and only in case of AV block would it start pacing the ventricle sequentially. Table 39.3 lists expected outcomes for each pacing mode. Dual-chamber PPM in DDD mode, with both chambers being monitored with the potential to be stimulated, is the most common PPM setup and typically achieves physiologic rhythm, except in the case of left bundle branch block. The absence of atrial sensing in DVI mode is designed for patients with intermittent atrial fibrillation. During periods of atrial fibrillation, the PPM works in VVI mode, but in sinus rhythm AV synchronization is achieved by dual-chamber pacing.
used. The first three letters specify the chamber(s) paced, the chamber(s) sensed, and the pacing algorithm (response to a sensed beat), respectively. The NBG code is summarized in Table 39.2. The choice of the specific pacemaker and its programming is adjusted to fit the patient needs. For example, in sick sinus syndrome, a dual-chamber PPM could be implanted with a DDD-backup mode programmed. Thus, the PPM would pace AAI and only in case of AV block would it start pacing the ventricle sequentially. Table 39.3 lists expected outcomes for each pacing mode. Dual-chamber PPM in DDD mode, with both chambers being monitored with the potential to be stimulated, is the most common PPM setup and typically achieves physiologic rhythm, except in the case of left bundle branch block. The absence of atrial sensing in DVI mode is designed for patients with intermittent atrial fibrillation. During periods of atrial fibrillation, the PPM works in VVI mode, but in sinus rhythm AV synchronization is achieved by dual-chamber pacing.
TABLE 39.1 Choice of Pacemaker Generator in Selected Indications for Pacing | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
In addition to the PPM mode, output energy and sensitivity can be adjusted. After the output threshold is determined by decreasing the energy to the minimum value needed to pace, the output energy is typically programmed to twice the threshold. Adjusting the sensitivity to a certain threshold is intended to eliminate sensing of electrical activity from T waves or other muscle potentials.
TABLE 39.2 The Pacemaker Code | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|