Percutaneous coronary intervention (PCI) for protected left main coronary artery (PLM) disease is complex because of patient and lesion factors; however, limited data exist on the outcomes of drug-eluting stent (DES) use for this indication. DEScover is a prospective observational study that enrolled consecutive patients with PCI in 2005. In-hospital and 1-year statuses were analyzed for 6,172 patients treated with DES according to LM and coronary artery bypass grafting (CABG) statuses (PLM, n = 93; previous CABG native vessel non-LM, n = 722; no previous CABG, n = 5,357). Cumulative event rates were calculated by the Kaplan–Meier method. Cox proportional hazards regression was used for multivariable analysis of adverse events. Baseline clinical, angiographic, and procedural variables differed significantly among groups, with patients with previous CABG, PLM, and non-LM having higher risk characteristics. In patients with previous CABG, after adjustment with CABG non-LM as a reference group, there were no significant differences in 1-year risk of any adverse event except a trend toward a greater risk of myocardial infarction (MI) in patients with PLM (adjusted hazard ratio 2.4, confidence interval 0.95 to 6.2, p = 0.06). However, patients after CABG (PLM and non-LM) compared to patients without previous CABG had a similar adjusted risk of death, MI, and stent thrombosis; an increased risk of target lesion revascularization (adjusted hazard ratio 1.79, confidence interval 1.2 to 2.6, p = 0.003), target vessel revascularization and death/MI/target vessel revascularization; and a lower risk of CABG (adjusted hazard ratio 0.25, confidence interval 0.09 to 0.67, p = 0.006). In conclusion, status after CABG rather than PLM location increases the risk of repeat revascularization with PCI in DES-treated patients.
Protected left main coronary artery (PLM) percutaneous coronary intervention (PCI) is often performed in patients with graft occlusion after coronary artery bypass grafting (CABG) because of the high perioperative morbidity and mortality associated with repeat bypass. LM lesions are complex owing to aorto-ostial location, calcification, and distal bifurcation involvement. In the bare-metal stent era, PCI of PLM and unprotected LM lesions had a high acute procedural success rate but restenosis resulted in repeat revascularization rates of 18% to 25% and there was a concerning high mortality in patients with unprotected LM lesions. Drug-eluting stents (DESs) have been studied in unprotected LM lesions and a meta-analysis of 1, 278 patients found a target vessel revascularization rate of 6.5% and a mortality of 5.5% at a median of 10 months. Patients with previous CABG, however, are a high-risk group and PCI of PLM lesions with DESs has not been well studied, cannot be extrapolated from the unprotected LM data, and can be considered untested. Compared to on-label indications for DESs, untested use is associated with a higher risk of target vessel revascularization. Given the lack of data on DES use in the PLM lesion subset, we used the DEScover registry to compare outcomes among the following 3 groups of patients treated with DESs: CABG with PLM lesions, CABG with native vessel non-LM lesions, and without previous CABG.
Methods
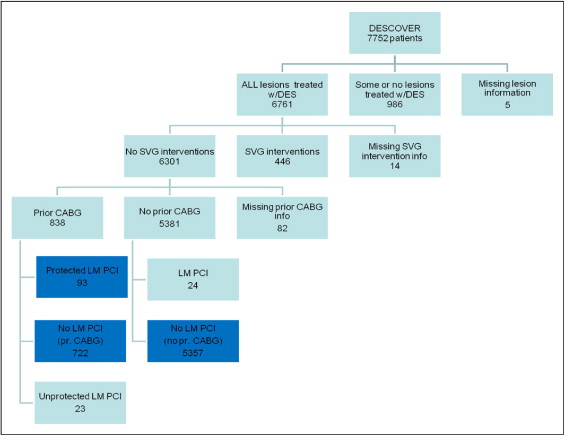
The DEScover is a prospective multicenter observational study designed to characterize patients with PCI from a broad sampling of hospitals and practices. Details of the study design have been previously described. In brief, from January through June 2005, 7,752 patients undergoing PCI were consecutively enrolled at 140 United States sites. Refusal or inability to provide written informed consent and/or Health Insurance Portability and Accountability Act authorization was the only exclusion criterion. This analysis includes data on 6,172 patients treated with DESs (sirolimus-eluting or paclitaxel-eluting stents) in 3 groups: no previous CABG non-LM (n = 5,357, group 1), previous CABG native vessel (n = 722, group 2; excludes LM and saphenous vein graft lesions), and PLM (n = 93, group 3). The remaining patients were excluded because not all lesions treated with DESs (n = 986), saphenous vein graft PCI (n = 446), missing CABG or lesion information (n = 101), and unprotected LM PCI (n = 47; Figure 1 ) . Baseline clinical, angiographic, and procedural informations were determined by site. Data were submitted through a secure Web site and follow-up was obtained by an independent service using a mail survey and/or telephone contact at 1 year. For those patients reporting an event, a specially trained research coordinator then obtained additional information. The University of Pittsburgh serves as the statistical analysis core. Follow-up was 89.6% complete at 1 year.
The definitions for “procedural success” and “myocardial infarction” (MI) have been previously described. Death is reported from any cause. Death and MI were not adjudicated. “Definite stent thrombosis” is defined as the presence of angiographic thrombus accompanied by an acute coronary syndrome. “Probable stent thrombosis” is defined as unexplained sudden cardiac death or Q-wave MI in the distribution of the stented artery when the stented segment was not known to be patent. An independent committee adjudicated events considered stent thrombosis. In this report, rates of stent thrombosis include those classified as definite or probable stent thrombosis. Repeat PCI was categorized according to whether the index lesion (target lesion revascularization) or artery (target vessel revascularization) was attempted. Coronary bypass grafting in the target vessel was included in the overall target vessel revascularization rate.
Differences in baseline, angiographic, and procedural characteristics and in-hospital outcomes were compared among the 3 patient groups by analysis of variance for continuous data and chi-square test for categorical variables. Cumulative 1-year adverse event rates were estimated by the Kaplan–Meier approach and compared by log-rank test. Patients lost to follow-up were censored at the last known date of contact. Comparisons at 1 year were made among the 3 groups and for each of 2 group pairings: no CABG and previous CABG non-LM (group 1 vs 2), no CABG and previous CABG PLM (group 1 vs 3), and previous CABG non-LM and PLM (group 2 vs 3). Cox proportional hazards regression was used for multivariate analysis of adverse events. Variables selected for adjustment were those significantly associated with the clinical outcome of interest or considered biologically relevant. Proportional hazards assumptions were evaluated and met. A p value <0.05 was considered statistically significant.
Results
There were statistically significant differences observed among the 3 groups of patients for all baseline factors ( Table 1 ). In general, patients with previous CABG were older, more likely men, and had more co-morbidities than the non-CABG group. Patients without previous CABG, however, were more likely current smokers and had acute MI as the indication for PCI.
| Variable | Non-LM PCI (no CABG) | Non-LM PCI (CABG) | Protected LM PCI (CABG) | p Value |
|---|---|---|---|---|
| (n = 5,357) | (n = 722) | (n = 93) | ||
| Age (years), mean ± SD | 63.1 ± 11.9 | 67.0 ± 10.8 | 66.7 ± 10.6 | <0.0001 |
| Men | 66.5% | 73.8% | 78.5% | <0.0001 |
| Hypertension | 72.9% | 81.0% | 86.0% | <0.0001 |
| Hypercholesterolemia ⁎ | 70.8% | 87.7% | 91.4% | <0.0001 |
| Diabetes mellitus | 29.5% | 37.8% | 38.7% | <0.0001 |
| Current smoker | 26.6% | 14.6% | 18.3% | 0.0002 |
| Previous myocardial infarction | 21.6% | 45.2% | 49.5% | <0.0001 |
| Previous percutaneous coronary intervention | 33.4% | 52.8% | 44.1% | <0.0001 |
| Heart failure | 7.9% | 17.3% | 18.3% | <0.0001 |
| Previous peripheral vascular disease | 7.0% | 14.5% | 17.2% | <0.0001 |
| Previous stroke | 4.3% | 6.0% | 7.5% | 0.046 |
| Clinical presentation | <0.0001 | |||
| Acute myocardial infarction without shock | 21.7% | 8.6% | 7.5% | |
| Unstable angina pectoris | 31.2% | 38.3% | 32.3% | |
| Stable angina pectoris | 13.8% | 19.0% | 17.2% | |
| Acute myocardial infarction with shock | 1.4% | 0.7% | 0.0% | |
| Positive ischemia | 24.4% | 24.8% | 36.6% | |
| Other | 7.5% | 8.6% | 6.5% |
Patients with previous CABG had a lower mean left ventricular ejection fraction and higher percent multivessel disease ( Table 2 ). In the PLM group compared to the post-CABG non-LM and no previous CABG groups, a larger number of lesions was attempted, multilesion PCI was more common, and a larger number of DESs was used. In addition, there was a higher prevalence of high-risk lesion subsets treated in the PLM group including ostial lesions, bifurcation lesions, and calcified lesions. Complete procedural success was high in all 3 groups but lower in the PLM group (complete success 98.7% of no-CABG group, 98.3% of CABG non-LM group, and 94.6% of PLM group, p = 0.004).
| Non-LM PCI (no CABG) | Non-LM PCI (CABG) | Protected LM PCI (CABG) | p Value | |
|---|---|---|---|---|
| (n = 5,357) | (n = 722) | (n = 93) | ||
| Number of coronary arteries narrowed ≥50% | <0.0001 | |||
| 1 | 61.1% | 40.8% | 24.1% | |
| 2 | 29.0% | 21.2% | 26.4% | |
| 3 | 9.9% | 38.0% | 49.4% | |
| Ejection fraction (%), mean ± SD | 53.6 ± 12.6 | 49.3 ± 13.6 | 47.6 ± 15.8 | <0.0001 |
| Number of narrowings attempted, mean ± SD | 1.5 ± 0.7 | 1.5 ± 0.8 | 1.8 ± 0.9 | <0.0001 |
| Multilesion intervention (≥2) | 34.9% | 35.7% | 57.0% | <0.0001 |
| Number of drug-eluting stents, mean ± SD | 1.4 ± 0.6 | 1.4 ± 0.7 | 1.7 ± 0.8 | <0.001 |
| Taxus | 41.6% | 45.3% | 47.3% | 0.10 |
| Cypher | 60.9% | 56.9% | 59.1% | 0.12 |
| Reference vessel diameter (mm), mean ± SD ⁎ | 3.0 ± 0.5 | 2.9 ± 0.5 | 3.1 ± 0.5 | <0.0001 |
| Lesion length (mm), mean ± SD ⁎ | 16.2 ± 9.8 | 16.8 ± 10.5 | 13.6 ± 8.5 | 0.0001 |
| Bifurcation lesion | 8.7% | 8.4% | 21.5% | <0.0001 |
| Calcified lesion | 21.9% | 32.0% | 45.2% | <0.0001 |
| Ostial lesion | 12.8% | 16.4% | 44.6% | <0.0001 |
| Total occlusion | 11.6% | 4.7% | 3.2% | <0.0001 |
| Any lesion complication | 5.6% | 5.7% | 10.8% | 0.10 |
| Complete procedural success | 98.7% | 98.3% | 94.6% | 0.004 |
| Hospital discharge medication | ||||
| Thienopyridine | 99.1% | 98.9% | 98.9% | 0.84 |
| Aspirin | 97.0% | 97.5% | 100.0% | 0.18 |
| β Blocker | 74.2% | 75.0% | 77.2% | 0.74 |
| 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors | 79.9% | 79.8% | 87.0% | 0.24 |
| Angiotensin-converting enzyme inhibitors | 44.9% | 45.3% | 55.4% | 0.13 |
In patients with previous CABG, 1-year outcomes for PLM versus non-LM PCI including death, death/MI, stent thrombosis, and target vessel revascularization were similar ( Table 3 ). There was a trend toward a higher rate of target lesion revascularization and a significantly higher rate of MI in the PLM compared to the non-LM CABG group. After adjustment ( Table 4 ) with CABG non-LM as a reference group, there were no significant differences in 1-year risk of any adverse event except a trend toward a greater risk of MI in patients with PLM remained.
| Total Patients (n = 6,172) | Group 1 Non-LM PCI (no CABG) (n = 5,357) | Group 2 Non-LM PCI (CABG) (n = 722) | Group 3 Protected LM PCI (CABG) (n = 93) | p Value | |||
|---|---|---|---|---|---|---|---|
| 1 vs 2 | 1 vs 3 | 2 vs 3 | |||||
| Death | 2.64% | 5.33% | 4.49% | <0.001 | <0.001 | 0.29 | 0.72 |
| Myocardial infarction | 1.97% | 2.76% | 6.67% | 0.003 | 0.15 | 0.001 | 0.05 |
| Stent thrombosis | 0.64% | 0.72% | 2.22% | 0.16 | |||
| Coronary bypass | 1.49% | 0.78% | 2.30% | 0.27 | |||
| Death/myocardial infarction | 4.40% | 7.61% | 10.04% | <0.001 | <0.001 | 0.009 | 0.42 |
| Target lesion revascularization | 2.71% | 4.50% | 9.47% | <0.001 | 0.008 | <0.001 | 0.06 |
| Target vessel revascularization | 5.54% | 7.54% | 10.61% | 0.02 | 0.03 | 0.04 | 0.35 |
| Death/myocardial infarction/target vessel revascularization | 8.75% | 13.94% | 17.15% | <0.001 | <0.001 | 0.006 | 0.46 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


