A growing number of solid organ transplant survivors require surgery for cardiac disease. We examined the effect of having a previous transplant on outcomes after cardiac surgery in these patients from a population-based perspective. Of 1,709,735 patients who underwent coronary artery bypass grafting, valve, or thoracic aorta surgery from 2004 to 2008 in the Nationwide Inpatient Sample, 3,535 patients (0.21%) had a previous organ transplant (2,712 kidney, 738 liver, 300 pancreas). Multivariate logistic regression analysis and propensity score matching were used to determine the effect of a previous solid organ transplant on outcomes. In-hospital mortality rate was 7% for patients who underwent transplantation versus 4% for patients who did not undergo transplantation (odds ratio [OR] 1.66, 95% confidence interval [CI] 1.16 to 2.38). Patients who underwent transplantation were at an increased risk for acute renal failure (OR 1.62, CI 1.36 to 1.94) and blood transfusions (OR 1.63, CI 1.36 to 1.95). Median length of stay was longer (10 vs 9 days), with greater median total charges ($111,362 vs $102,221; both p <0.001). Occurrence of stroke, gastrointestinal complication, infection, and pneumonia was similar between groups. In conclusion, previous solid organ transplantation is an incremental risk factor for postoperative mortality after cardiac surgery. Renal protective strategies and bleeding control should be stressed to mitigate complications.
The prevalence of solid organ transplant recipients with functioning allografts continues to increase over time. Renal and hepatic transplants account for most annual transplantations, and these patients carry with them an increased risk for cardiovascular disease greater than the general population. Traditional cardiovascular risk factors such as hypertension, hyperlipidemia, and metabolic syndrome are more prevalent in patients undergoing transplantation and exacerbated by immunosuppressive drugs. Dialysis-dependent time before kidney transplant and poor renal graft function has been associated with the increased risk for coronary heart disease. Cardiovascular events are among the most common causes of late death in the transplant recipient population. Accordingly, there is an increasing number of surviving solid organ transplant recipients requiring cardiovascular intervention. The aim of this study was to examine trends and characteristics of patients with previous solid organ transplant undergoing cardiac surgery, and the impact of previous transplant on mortality, complications, and resource utilization.
Methods
Data were obtained from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (NIS) database from 2004 to 2008. The NIS is a 20% stratified sample of all discharges occurring in a given year from approximately 1,000 US hospitals in 32 to 37 states (depending on the year of the study). Discharge weights are provided, which allow extrapolation to nation-level estimates from the unweighted database information. Weighted estimates are reported throughout this study.
Data on 1,709,735 adult patients who underwent cardiovascular surgery were identified by International Classification of Diseases, Ninth Version, Clinical Modification (ICD-9-CM) procedure codes for coronary artery bypass grafting (CABG, 36.1x), valve repair or replacement (35.1x, 35.2x), or thoracic aortic surgery (38.45). Of these, patients with a history of solid organ transplant were identified using ICD-9-CM diagnosis codes: V42.0 (kidney), V42.7 (liver), and V42.83 (pancreas). The patients who underwent cardiac surgery without transplant ICD-9-CM coding were used as a comparison group. Patients with heart transplant coding V42.1 were excluded from this study, as were patients younger than 18 years or older than 100 years. There were 3,535 patients (0.21%) meeting these criteria, 2,712 kidney, 738 liver, and 300 pancreas.
The outcomes analyzed for each hospitalization were in-hospital mortality, length of stay, discharge disposition, hospital charges and cost, and complications. The complications were identified through secondary ICD-9-CM coding and included stroke (997.0, 430, 431, 432, 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91, 436, 438.0, 438.10, 438.11, 438.12, 438.19, 438.2, 438.3, 438.4, 438.5, 438.81, 438.82, 438.89, 438.9), tamponade (423.0, 423.3, 37.0), blood transfusion (99.02, 99.04), infection (998.5), acute renal failure (584), pneumonia (481, 482, 485, 486, 507), gastrointestinal complication (997.4), graft rejection (996.8, in patient group who underwent transplantation only), and the composite outcome of any complication. The categories of disposition were routine discharge, transfer to another inpatient facility, transfer to another type of facility (including acute care or skilled nursing facilities), and home health care. Hospital resource consumption was evaluated by hospitalization charges and cost, both reported in 2008 US dollars. Total charges do not include professional fees, and total costs are derived from total charges using a cost-to-charge ratio created by Healthcare Cost and Utilization Project that is based on accounting reported from the Centers for Medicare and Medicaid Services.
Demographics, co-morbidities, insurance status, hospital characteristics, and the region where procedure were performed were considered. Patient-level variables included age, gender, race, and insurance status. Race or ethnicity was categorized as White, Black Hispanic, and other/missing. Insurance status was categorized as Medicare, Medicaid, private insurance, uninsured, and other. The co-morbidities for risk adjustment were derived from the secondary ICD-9-CM diagnosis codes using the Deyo modification of the Charlson co-morbidity Index. A hospital was considered to be a teaching hospital if it had a residency program approved by the American Medical Association, was a member of the Council of Teaching Hospitals, or had a ratio of full-time equivalent interns and residents to beds of 0.25 or higher. Hospital region was classified as Northeast, Midwest, South, or West by the US Census Bureau. The surgical procedure was categorized as isolated CABG, isolated valve repair or replacement, isolated aortic surgery, or a combination of 2 or more of these.
The mean, median, and standard deviation were calculated for all continuous outcomes, and frequency counts and percentages for categorical outcomes. To compare differences by transplant status we used the chi-square test for categorical variables and the t test and Wilcoxon–Mann–Whitney test for continuous variables. For descriptive and unadjusted analysis, we used discharge-level survey weights provided in the NIS and accounted for complex survey design effects using the appropriate procedures in the SAS software (e.g., SURVEYFREQ and SURVEYMEANS, SAS/STAT Software, version 9.3 (2011) by SAS Institute Inc., Cary, North Carolina). We used a Mann–Kendall nonparametric test to test if the annual percentage of patients who underwent cardiac surgery with a previous transplant has changed over time.
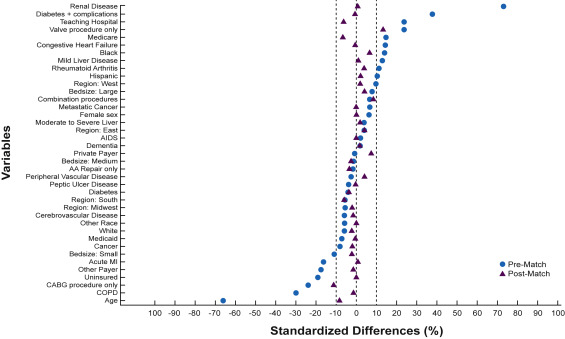
We used propensity score matching to balance the covariables for patients with and without previous transplant to assess outcomes without influence from known factors. Propensity scores, or the conditional probability of having a history of previous solid organ transplant, were estimated for each patient using a multivariate logistic regression model. In this model, the presence of previous transplant was the dependent variable, and the patient demographics, payer status, co-morbidities, hospital characteristics, and procedure type were the independent variables. To match those with and without previous transplant, a 1:3 greedy matching algorithm with a caliper of 0.2 times the standard deviation of the linear propensity score. The balance of covariables before and after matching was assessed by calculating the standardized differences between those with and without previous transplant. Propensity matching resulted in 719 quartets of patients containing 1 patient with previous transplant and 3 patients without previous transplant who were well matched with respect to demographics, co-morbidities, and institutional characteristics ( Figure 1 ).
In addition to the main analysis, we sought to identify risk factors associated with death in patients who underwent transplantation using multivariate logistic regression. Owing to concerns of overparameterization, we used a stepwise approach to identify significant risk factors from the covariables mentioned previously; however, variables with small cell counts (n < 5) in either the alive or dead group were excluded from consideration as they produce unstable parameter estimates. The excluded variables were the co-morbidities of dementia, moderate to severe liver disease, hemiplegia, AIDS, and metastatic cancer, and the complications of tamponade, wound infection, and gastrointesitnal complications. We experimented with different entry and retention parameters, but settled on a low barrier to entry of 0.30 to allow more variables a chance to enter, but a strict 0.05 cutoff for retention in the final model, again due to concerns of overparameterization. For each of the considered variables, we also calculated the unadjusted odds ratio using simple logistic regression. Of the patients who underwent transplantation who had CABG, we investigated the effect of on-pump versus off-pump CABG using multivariate logistic regression for complication and mortality outcomes and multivariate linear regression for charge and length of stay outcomes. We controlled for all covariables mentioned earlier.
Results
Over the study period, the yearly incidence of solid organ transplant recipients undergoing cardiac surgery significantly increased (p = 0.027; Figure 2 ). Comparisons of demographic data and co-morbidites for patients with and without previous transplant are presented in Tables 1 and 2 . Previously transplanted patients had proportionately fewer isolated CABG operations (59% vs 70%), but more isolated valve (25% vs 16%) and combination surgeries (15% vs 13%, all p ≤0.001) than patients who did not undergo transplantation ( Figure 3 ). Operations by transplant organ type are provided in Table 3 .
| Characteristic | Previous Transplant | P | |
|---|---|---|---|
| Yes (n = 3535) | No (n = 1,705,949) | ||
| Age group (years) | <0.001 | ||
| 0-44 | 373 (11%) | 76,639 (5%) | |
| 45-54 | 895 (25%) | 226,907 (13%) | |
| 55-64 | 1267 (36%) | 443,724 (26%) | |
| 65-74 | 784 (22%) | 524,328 (31%) | |
| ≥ 75 | 216 (6%) | 434,350 (25%) | |
| Mean age, years ± SD | 58.2 ± 10.5 | 65.5 ± 11.8 | <0.001 |
| Sex | 0.101 | ||
| Male | 2322 (66%) | 1,166,310 (68%) | |
| Female | 1213 (34%) | 539,337 (32%) | |
| Race/ethnicity | <0.001 | ||
| White | 2025 (57%) | 1,019,746 (60%) | |
| Black | 278 (8%) | 77,769 (4%) | |
| Hispanic | 255 (7%) | 80,799 (5%) | |
| Other/missing | 977 (28%) | 527,518 (31%) | |
| Primary payer | <0.001 | ||
| Medicare | 119 (3%) | 82,029 (5%) | |
| Medicaid | 2161 (61%) | 918,923 (54%) | |
| Private | 1213 (34%) | 598,797 (35%) | |
| Other | 23 (1%) | 52,766 (3%) | |
| Uninsured | 19 (1%) | 52,967 (3%) | |
| Hospital Region | 0.050 | ||
| Northeast | 710 (20%) | 316,389 (18%) | |
| Midwest | 779 (22%) | 417,096 (23%) | |
| South | 1300 (37%) | 680,229 (41%) | |
| West | 746 (21%) | 292,235 (18%) | |
| Teaching Status | <0.001 | ||
| Non-Teaching | 1005 (29%) | 672,398 (40%) | |
| Teaching | 2531 (71%) | 1,033,551 (60%) | |
| Hospital bed size | 0.081 | ||
| Small | 144 (4%) | 107,529 (7%) | |
| Medium | 659 (19%) | 328,377 (19%) | |
| Large | 2732 (77%) | 1,270,044 (74%) | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


