Organizing Pneumonia
Allen P. Burke, M.D.
Teklu Legesse, M.D.
Terminology
Organizing pneumonia (OP) is a histologic “pattern” that denotes a subacute phase of lung injury characterized by loose fibrosis that is reasonably discrete and circumscribed.1 The term “BOOP” (bronchiolitis obliterans organizing pneumonia) is used by some2 and discouraged by others.3 The true frequency of bronchiole-related OP may be underestimated due to sampling or sectioning artifact, but it seems fairly certain that a large proportion of OP occurs in the interstitium remote from the airways, favoring the term “OP” over “BOOP.” Idiopathic OP is termed “cryptogenic organizing pneumonia” or “idiopathic BOOP” and is discussed in Chapter 19. OP or BOOP should not be confused with obliterative bronchiolitis, bronchiolitis obliterans syndrome, or constrictive bronchiolitis (see Chapter 37), all of which are immunerelated airway destructive processes and histologically distinct from OP.
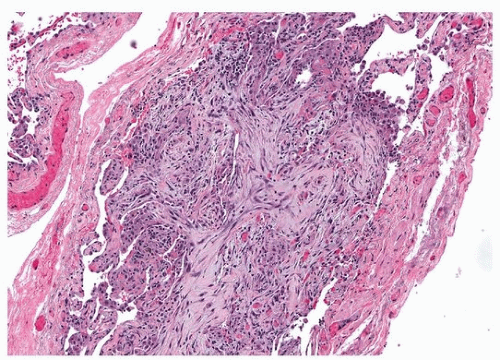
Microscopic Findings
OP is characterized by nodules of myofibroblasts within a background of extracellular matrix and collagen (Fig. 5.1). These nodules are sometimes called “Masson bodies,” a term ascribed to Masson years after he published histologic findings of the lungs of patients with acute rheumatic fever.4 OP is either within the bronchioles (“polypoid bronchiolitis obliterans”) (Fig. 5.2), adjacent to the bronchioles (Fig. 5.3), or within the interstitium. If there is coalescence into a nodule, or if airways are not readily identified, relationship to airway is indeterminate (Fig. 5.4). There may be associated granulomas adjacent to or within the organizing pneumonia (Fig. 5.5). Fibrin is occasionally present, in which case, the term “acute and organizing pneumonia” may be used. Granulation tissue may occur, but usually, the lesion is often composed almost completely of fibroblasts, ground substance, and chronic inflammation, with little neovascularity. There may be focal reactive pneumocyte hyperplasia, but widespread pneumocyte changes with diffuse interstitial loose fibrosis are more typical of diffuse alveolar damage than OP (Fig. 5.6). There may be adjacent interstitial inflammation, especially in hypersensitivity pneumonitis, as well as adjacent fibrosis, with an NSIP-like pattern, especially in COP.
Differential Diagnosis
The OP “pattern” is invariable in cryptogenic organizing pneumonia and organizing infectious or aspiration pneumonia (Figs. 5.7 and 5.8). It is typically seen as a component of hypersensitivity pneumonitis, drug-induced lung injury, autoimmune lung injury such as rheumatoid lung disease, alloimmune lung injury, and allergic lung injury ( eosinophilic pneumonia) (Table 5.1). OP may be present to a lesser degree in virtually any condition with lung injury, including Wegener granulomatosis, pneumoconiosis, ECMO-related lung injury, and NSIP. OP is a characteristic of “acute fibrinous and organizing pneumonia,” a recently described interstitial lung disease that is a variant of acute interstitial pneumonia (see Chapter 19). OP may be present in areas of lung not grossly involved by honeycombing in idiopathic pulmonary fibrosis (UIP). Areas of OP are frequently seen in patients with emphysema (Fig. 5.9), and adjacent to tumors, presumably
by a variety of mechanisms including obstruction and infection. OP may be the only finding in masses resected from patients with suspected neoplasms, especially in those with known cancers who are being investigated for possible metastatic disease. In these cases, OP is likely the consequence of an infectious or obstructive process.
by a variety of mechanisms including obstruction and infection. OP may be the only finding in masses resected from patients with suspected neoplasms, especially in those with known cancers who are being investigated for possible metastatic disease. In these cases, OP is likely the consequence of an infectious or obstructive process.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree