Open Surgery for Descending Aortic Lesions
Yutaka Okita
Shinichi Takamoto
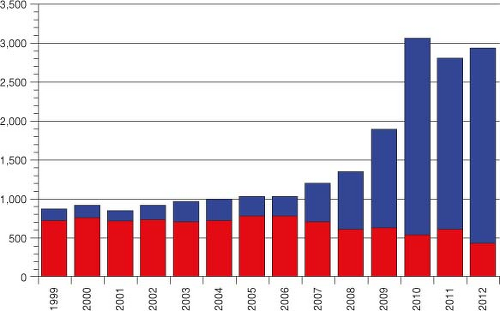
Since the introduction of thoracic endovascular aortic repair (TEVAR) for treatment of thoracic aortic aneurysms, the number of open surgeries for nondissecting aortic aneurysms of the descending aorta has decreased steeply. This is because TEVAR is less invasive and is associated with secure exclusion of the aneurysm, and a decreased incidence of spinal cord complications. According to the annual survey by the Japanese Association for Thoracic Surgery, the number of open surgeries for nondissecting aneurysm of the descending aorta was 722, and the number of TEVARs for this lesion was 140 in 1999. By contrast, in 2012, the number of open surgeries was 427 and the number of TEVARs was 2,505 (Fig. 13.1). However, there remains a need for open thoracotomy in patients in whom TEVAR is inappropriate, such as those with mega-aorta syndrome with no landing zone for a stent graft, those with poor iliac access to the aorta, those who have failed TEVAR, and those with infective aortic lesions.
There are several contraindications for open surgery for management of descending aortic aneurysms. For example, patients with severe chronic obstructive lung disease (COPD) usually have severe adhesions of the left lung to the aorta, and surgical manipulation causes significant lung damage, which can lead to postoperative disability. Advanced age, comorbidities involving the vital organs, and severe frailty are other potential reasons to avoid open surgery.
A multidisciplinary team approach is essential to establish the optimal strategy for treatment of descending aortic aneurysms. A team conference including surgeons, cardiologists, radiologists, perfusionists, and anesthesiologists is held weekly in our institute where management decisions are made (e.g., open surgery, endovascular intervention, or medical treatment). A preoperative sheet is made to describe the patients’ history, present
status, and cardiac, pulmonary, cerebral, biochemical, and hematologic data with computed tomography (CT), angiography, and magnetic resonance (MR) images.
status, and cardiac, pulmonary, cerebral, biochemical, and hematologic data with computed tomography (CT), angiography, and magnetic resonance (MR) images.
On the day before surgery a 5-Fr silicone catheter is introduced into the subarachnoid space for continuous drainage of cerebrospinal fluid for spinal cord protection.
Approach and Exposure
Normally, patients are positioned in the right semirecumbent position (left side up). Before establishing the tilting position, right and left groin incisions are made in the supine position to expose the right common femoral vein and the left common femoral artery for cardiopulmonary bypass (CPB). In the right semirecumbent position, a 16-gauge Tuohy needle with a 5-Fr catheter for regional nerve block is inserted from the subscapular area to the paravertebral space and another Tuohy needle is introduced from the L2-L3 intervertebral space.
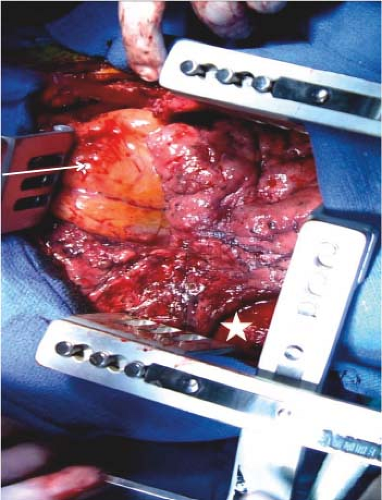
A posterolateral oblique skin incision is made from the subscapular region to the left submammary area. The muscles are divided with meticulous hemostasis. The left pleural cavity is entered through the fourth intercostal space for lesions in the distal arch to the proximal descending aorta. For distal descending aortic aneurysms, the chest is opened through the sixth intercostal space. For extensive lesions, such as those extending from the distal arch to the diaphragm, rib-cross thoracotomy is preferred by usually transecting one or two ribs posteriorly. Two large (29-cm) Burford–Finochietto type rib retractors (Geister, Tuttlingen, Germany) are used and set in a crossed position (Fig. 13.2). Unilateral ventilation to minimize injury of the left lung from surgical manipulation and to improve exposure is utilized when possible. The left lung should always be wrapped by a moist pad.
Aortic Control
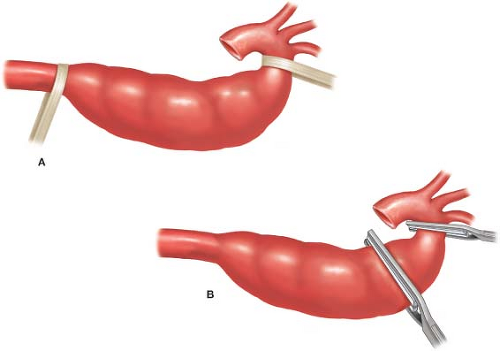
Umbilical tapes are passed around the aorta proximal and distal to the aneurysm, except for patients in whom the proximal aortic clamp is not utilized. Dissection of the aorta should be performed while avoiding injury to the neighboring vital organs,
such as the esophagus, thoracic duct, hemiazygos vein, sympathetic trunk, and vagal nerve (Fig. 13.3A).
such as the esophagus, thoracic duct, hemiazygos vein, sympathetic trunk, and vagal nerve (Fig. 13.3A).
Arterial Cannulation and Venous Drainage
The left common femoral artery is usually used for arterial return. A 20- to 22-Fr thin-wall cannula (Medtronic, Edwards) is sufficiently large for partial CPB or total CPB in a normal-sized patient. On rare occasions, the left axillary artery is selected for additional
inflow. In patients with a shaggy atherosclerotic aorta, the axillary artery is also cannulated and perfused in order to minimize debris embolization to the brain due to retrograde arterial perfusion.
inflow. In patients with a shaggy atherosclerotic aorta, the axillary artery is also cannulated and perfused in order to minimize debris embolization to the brain due to retrograde arterial perfusion.
For venous drainage, a 24- to 27-Fr long venous cannula with multiple side holes (Medtronic, Edwards) is inserted into the right common femoral vein. A distance of 45 to 50 cm insertion from the right femoral vein puncture site usually places the tip of the cannula into the right atrium. When venous drainage is not sufficient or when total bypass is required, an additional 24- to 28-Fr venous cannula is inserted in the left pulmonary artery after pericardiotomy.
Anastomosis
As soon as sufficient blood flow to the distal body is obtained, the proximal aorta is clamped to prevent retrograde embolization. The second clamp is applied at 5 to 10 cm below the first clamp and perfusion of the lower body is maintained (Fig. 13.3B). The aorta between the clamps is transected completely, and dissection is performed between the aortic adventitia and the esophagus, left recurrent or vagal nerve, and azygos vein.
The exclusion technique to anastomose the aorta with a Teflon felt strip reinforcement should be used in order to prevent injury to the esophagus. Full-thickness bites are performed using 4-0 monofilament sutures with 22-mm needles. The distal anastomosis to the aorta is performed in a similar fashion (Fig. 13.4A to E).
A branched woven Dacron gelatin sealed graft (J graft Japan Life Line) or a triple-layered graft (Triplex, Terumo) is the preferred graft.
Proximal Open Anastomosis During Retrograde Cerebral Circulation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree