INDICATIONS/CONTRAINDICATIONS
Open cricopharyngeal myotomy is indicated in any patient in whom significant oropharyngeal dysphagia is documented. Aspiration, regurgitation, and weight loss are also common presenting symptoms. As the difficulty in swallowing is at the confluence of the esophageal opening and the tracheobronchial tree, the surgeon needs to be ready to manage persistent aspiration by laryngeal exclusion or excision. Relative contraindications to the operation are dictated by the medical condition of the patient. Recently, some surgeons have advocated transoral stapling in patients with significant medical comorbidities.

Figure 18.1 Radiographic image of a Zenker’s diverticulum.
Etiology
 Neurologic
Neurologic
 Myogenic
Myogenic
 Iatrogenic
Iatrogenic
 Idiopathic
Idiopathic
 UES dysfunction alone
UES dysfunction alone
 UES dysfunction with pharyngoesophageal diverticulum
UES dysfunction with pharyngoesophageal diverticulum
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
 Clinical assessment of symptoms. Assessment of clinical symptoms is essential as they are the main reason for the intervention. Quantification of the symptoms by a scoring system or by the patient on a numerical scale is seen as an objective index of symptom severity with the advantage of allowing post-treatment assessment.
Clinical assessment of symptoms. Assessment of clinical symptoms is essential as they are the main reason for the intervention. Quantification of the symptoms by a scoring system or by the patient on a numerical scale is seen as an objective index of symptom severity with the advantage of allowing post-treatment assessment.
 Videoradiology of the pharyngoesophageal junction. Videoradiology is an important method of investigation, as it describes the very rapid events that occur with swallowing. The documentation of abnormal sphincter opening, of laryngeal competence, and of the type and size of the herniated pouch is important for planning the type of operation to be offered. Distal esophageal pathology must be ruled out.
Videoradiology of the pharyngoesophageal junction. Videoradiology is an important method of investigation, as it describes the very rapid events that occur with swallowing. The documentation of abnormal sphincter opening, of laryngeal competence, and of the type and size of the herniated pouch is important for planning the type of operation to be offered. Distal esophageal pathology must be ruled out.
 Radionuclide quantification of emptying. Radionuclide scintigrams are used to quantify bolus retention before surgery and the improved clearance after treatment. Manometric studies help to understand the pathophysiology of the condition. They require strict interpretation criteria. The presence of symptoms without any evidence of abnormality on investigation must raise doubts regarding the indication for surgical treatment.
Radionuclide quantification of emptying. Radionuclide scintigrams are used to quantify bolus retention before surgery and the improved clearance after treatment. Manometric studies help to understand the pathophysiology of the condition. They require strict interpretation criteria. The presence of symptoms without any evidence of abnormality on investigation must raise doubts regarding the indication for surgical treatment.

Figure 18.2 Incision following the anterior border of the left sternomastoid muscle and extending from the sternal notch to a few centimetres from the ear lobe.
 SURGERY
SURGERY
General Principles
 Myotomy is the essential part of treatment to remove the restrictive dysfunction.
Myotomy is the essential part of treatment to remove the restrictive dysfunction.
 Treatment of the diverticulum is seen as managing the complication of the dysfunction.
Treatment of the diverticulum is seen as managing the complication of the dysfunction.
 Minute diverticula disappear with the myotomy.
Minute diverticula disappear with the myotomy.
 1- to 3-cm diverticula are suspended.
1- to 3-cm diverticula are suspended.
 Diverticula larger than 4 cm are resected.
Diverticula larger than 4 cm are resected.
Surgical Technique
 The patient lies supine with a pillow under the shoulders. The head is in hyperextension, rotated toward the right. The incision follows the anterior border of the left sternomastoid muscle and extends from the sternal notch to a few centimetres from the ear lobe (Fig. 18.2).
The patient lies supine with a pillow under the shoulders. The head is in hyperextension, rotated toward the right. The incision follows the anterior border of the left sternomastoid muscle and extends from the sternal notch to a few centimetres from the ear lobe (Fig. 18.2).
 The plane of access to the pharyngoesophageal junction must be developed anterior to the carotid artery and the deep jugular vein, just lateral and posterior to the thyroid gland (Fig. 18.3).
The plane of access to the pharyngoesophageal junction must be developed anterior to the carotid artery and the deep jugular vein, just lateral and posterior to the thyroid gland (Fig. 18.3).

Figure 18.3 Anatomic structures in the access plane.
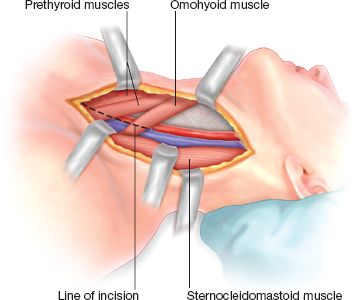
Figure 18.4 Exposed sternomastoid, omohyoid, and prethyroid muscles after division of the subcutaneous tissues and platysma.
 Subcutaneous tissues and platysma are divided first. A branch of the cervical cutaneous nerve traverses the incision, often in its middle or proximal part, and must be divided for proper exposure; submandibular cutaneous anaesthesia results. The sternomastoid muscle is dissected free and the omohyoid and the prethyroid muscles are exposed. They are divided along the incision line, freeing the thyroid gland (Fig. 18.4).
Subcutaneous tissues and platysma are divided first. A branch of the cervical cutaneous nerve traverses the incision, often in its middle or proximal part, and must be divided for proper exposure; submandibular cutaneous anaesthesia results. The sternomastoid muscle is dissected free and the omohyoid and the prethyroid muscles are exposed. They are divided along the incision line, freeing the thyroid gland (Fig. 18.4).
 Traction is exerted on the thyroid gland by the assistant. The middle thyroid vein is located and ligated. The deep cervical fascia is then under tension, and it is opened and divided progressively along the line of the incision. The inferior thyroid artery is identified and ligated just under the fascia (Fig. 18.5). Occasionally, the vascular supply to the superior pole of the thyroid must be ligated for proper exposure of the pharynx and hypopharynx.
Traction is exerted on the thyroid gland by the assistant. The middle thyroid vein is located and ligated. The deep cervical fascia is then under tension, and it is opened and divided progressively along the line of the incision. The inferior thyroid artery is identified and ligated just under the fascia (Fig. 18.5). Occasionally, the vascular supply to the superior pole of the thyroid must be ligated for proper exposure of the pharynx and hypopharynx.
 The cellular plane between the buccopharyngeal fascia and the prevertebral fascia is freed progressively and the whole pharyngoesophageal junction can be lifted and everted toward the surgeon. The pharyngoesophageal diverticulum develops between the cricopharyngeus, the cervical esophagus muscularis, and the buccopharyngeal fascia. The buccopharyngeal fascia must be divided, usually with the use of diathermy, to free the diverticulum (Fig. 18.6).
The cellular plane between the buccopharyngeal fascia and the prevertebral fascia is freed progressively and the whole pharyngoesophageal junction can be lifted and everted toward the surgeon. The pharyngoesophageal diverticulum develops between the cricopharyngeus, the cervical esophagus muscularis, and the buccopharyngeal fascia. The buccopharyngeal fascia must be divided, usually with the use of diathermy, to free the diverticulum (Fig. 18.6).

Figure 18.5 Deep cervical fascia is divided along the line of the incision.



