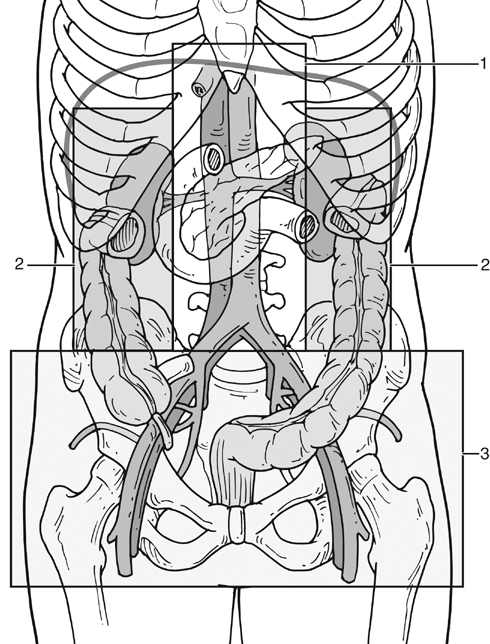
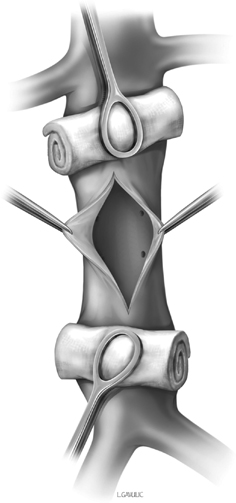
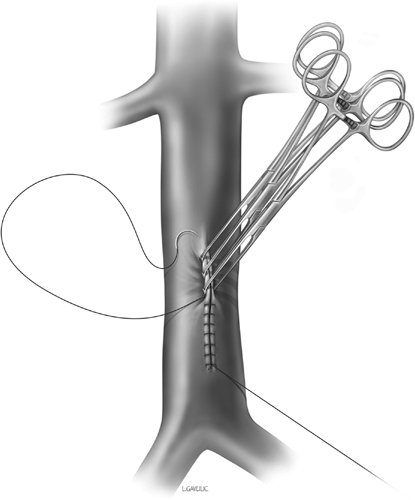
Most major vascular structures within the abdomen are retroperitoneal, and therefore the retroperitoneal zone that contains them can also aid in understanding basic management paradigms. There are three retroperitoneal zones (Figure 1). Major injury to the inferior vena cava (IVC) is a highly lethal event, especially when involving the retrohepatic region. Surgical treatment has primarily involved open techniques. Compression of the vena cava proximally and distally is an important part of hemorrhage control, with sponge-sticks being a useful adjunct in this regard (Figure 2). Even with adequate compression, hemorrhage can be significant as a result of renal and lumbar venous bleeding. The surgeon must be ready to make the initial repair the definitive repair, because suture laceration of the vein can easily convert a manageable injury to one that is complex or stellate. Allis clamps can aid in the repair of linear caval injuries and facilitate suture placement in a relatively bloodless field (Figure 3). Lacerations and puncture wounds should be sutured using permanent monofilament suture. The author recommends 4–0 nonabsorbably polypropylene monofilament (Prolene) suture on an SH needle, which may be manually straightened to lengthen the throw on the needle and enhance control. Using Teflon felt or skeletal muscle pledgets can aid in hemostasis if the vein wall is friable or if initial suture attempts pull through the vein wall.
Open and Endovascular Management of Blunt and Penetrating Nonaortic Abdominal Vascular Injury
Zones of Injury
Vena Cava Injuries
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


