Introduction
Chronic kidney disease (CKD) is associated with an increased risk of cardiovascular morbidity and mortality. CKD patients have advanced arterial wall stiffening. However, there is paucity on the association between abnormal levels of parathyroid hormone (PTH) and aortic stiffness in patients with CKD. In this study, we aimed to investigate the relationship between PTH levels and aortic stiffness calculated by echocardiography in patients with CKD.
Material and Methods
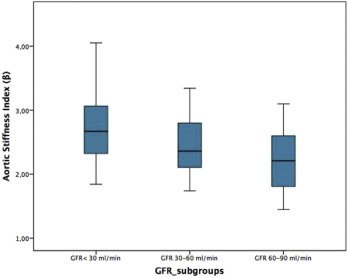
A total of 60 patients diagnosed as CKD were retrospectively evaluated. Patients were divided into 3 groups according to their eGFR values (< 30 mL/min, 30-60 mL/min and 60-90 mL/min). Basal demographical, clinical data and laboratory findings were compared between 3 groups. Transthoracic echocardiography was performed; all data were digitally stored and analyzed offline. The percentage change of the aortic root was calculated as the “aortic strain”; relative change in diameter for a given pressure change was calculated as “aortic distensibility” and ratio of ln(systolic/diastolic pressures) to (relative change in diameter) was calculated as aortic stiffness index (β). Biochemical marker data were obtained from the patients’ medical records via the hospital’s computerized database. The eGFR was measured using the 6 variable modifications of diet in renal disease (MDRD) equation.
Material and Methods
A total of 60 patients diagnosed as CKD were retrospectively evaluated. Patients were divided into 3 groups according to their eGFR values (< 30 mL/min, 30-60 mL/min and 60-90 mL/min). Basal demographical, clinical data and laboratory findings were compared between 3 groups. Transthoracic echocardiography was performed; all data were digitally stored and analyzed offline. The percentage change of the aortic root was calculated as the “aortic strain”; relative change in diameter for a given pressure change was calculated as “aortic distensibility” and ratio of ln(systolic/diastolic pressures) to (relative change in diameter) was calculated as aortic stiffness index (β). Biochemical marker data were obtained from the patients’ medical records via the hospital’s computerized database. The eGFR was measured using the 6 variable modifications of diet in renal disease (MDRD) equation.
Results
CKD patients with lower eGFR values have decreased aortic strain and aortic distensibility index and increased aortic stiffness index values compared with higher eGFR values. In univariate correlation analysis, PTH (r=0.338, p=0.009), LVIDd (r=0.263, p=0.044), age (r=0.374, p=0.003), history of diaebetes mellitus (r=0.407, p=0.001), eGFR (r=-0.384, p=0.003) and serum glucose level (r=0.367, p=0.004) significantly correlated with aortic stiffness index (β). Afterwards, we performed a standard multivariate regression analysis using the backward method to determine the independent association based on variables significantly differed between groups and significantly correlated in univariate correlation analysis (PTH, eGFR, IVSd, LVIDd, DM, serum glucose level, age, hemoglobin, Ca x phosphate). In multivariate linear regression analysis, serum level of PTH, history of diabetes mellitus and age were found as independent predictor of aortic stiffness index (β) in CKD patients.
Conclusion
The findings indicate a possible link between elevated PTH level and aortic stiffness index might be helpful the underlying pathophysiological mechanism of cardiovascular disease in patients with CKD.