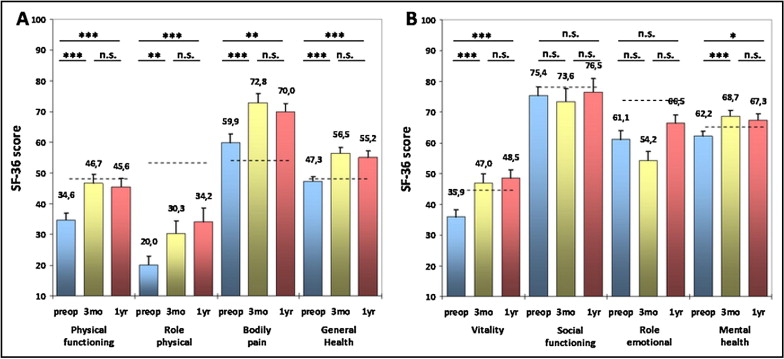
Recently, it has been demonstrated that transcatheter aortic valve implantation (TAVI) can result in significant improvement in patients’ quality of life (QOL) in the short term. At present, however, little is known about the long-term improvements in QOL after TAVI. Thus, our aim was to prospectively assess the 1-year QOL outcome of patients undergoing TAVI. We performed a prospective analysis of 186 patients with symptomatic severe aortic valve stenosis ineligible for conventional aortic valve replacement, who underwent TAVI with either the Medtronic CoreValve or Edwards Sapien device. A total of 106 patients completed the 1-year follow-up protocol. The QOL was measured using the Medical Outcomes Study 36-item short-form health survey questionnaire at baseline and at 3 months and 1 year of follow-up. At 1 year of follow-up, significant improvements in the Medical Outcomes Study 36-item short-form health survey questionnaire scores for physical functioning (baseline 34.6 ± 2.3 vs 1 year of follow-up 45.6 ± 2.7; p <0.001), role physical (20 ± 3.0 vs 34.2 ± 4.4; p <0.001), bodily pain (59.9 ± 3 vs 70 ± 2.7; p <0.01), general health (47.3 ± 1.5 vs 55.2 ± 2.1, p <0.001), vitality (35.9 ± 2 vs 48.5 ± 2; p <0.001), and mental health (62.2 ± 2.2 vs 67.3 ± 1.8; p <0.05) were observed compared to baseline. No significant improvement could be detected for social functioning (75.4 ± 2.5 vs 76.5 ± 2.6; p = 0.79) and role emotional (61.1 ± 4.3 vs 66.5 ± 4.7; p = 0.29). At 1 year of follow-up, the various physical and mental scores were comparable to an age-matched standard population. In conclusion, the present study has demonstrated that TAVI can improve the QOL status of high-surgical risk patients with severe aortic valve stenosis that can be maintained for ≤1 year postproceduraly in survivors. Although the mental subscales improved slightly, the mental component summary score failed to reach statistical significance in our study population.
Transcatheter aortic valve implantation (TAVI) has been developed as an alternative treatment modality for those patients in whom the surgical risk of conventional surgical aortic valve replacement is very high or prohibitive. TAVI has rapidly gained clinical acceptance during recent years, and it has been demonstrated that good short- and mid-term survival rates can be achieved. Beyond mortality and hemodynamic valve performance, the quality-of-life (QOL) dynamics have to be assessed to guide patient-centered clinical decision-making but also to judge the outcome of this novel and promising technology. Recently, we and others have demonstrated that TAVI can result in significant QOL improvement in the short term. Less is known about the QOL dynamics after TAVI in the longer term. Accordingly, we prospectively examined in 186 TAVI patients, how much TAVI is associated with an improvement in the physical and/or mental health scales at 1 year of follow-up using the Medical Outcomes Study 36-item short-form health survey questionnaire (SF-36).
Methods
Patients with severe, symptomatic aortic valve stenosis (effective orifice area <0.8 cm 2 , mean gradient >40 mm Hg, or peak aortic jet velocity >4.0 m/s) who were refused for surgical aortic valve replacement were evaluated for TAVI. Computed tomography of the chest, abdomen, and pelvis was performed in all patients to assess the anatomy of the complete aorta and to verify the suitability of the peripheral vessels for transfemoral access. The prosthesis type was chosen according to the measurements of the aortic root anatomy (native annulus diameter, sinus height, sinus width, ascending aortic diameter) using transthoracic/transesophageal echocardiography and/or computed tomography. Our policy was to consider the transfemoral site as the access of first choice. Only patients unsuitable for transfemoral implantation underwent subclavian or transapical TAVI.
For our prospective cohort study, we included all consecutive patients undergoing TAVI at the German Heart Center, Munich from November 2007 to December 2009. The inclusion criterion for participation was the ability to understand, read, and write German. Patients with language barriers were excluded. Study participation was voluntary. All patients provided written informed consent. The local ethics committee of the Technische Universität München approved the study (project number 2234/08).
QOL was assessed using the SF-36. All patients completed a baseline questionnaire after admission to the hospital 1 day before the intervention. At 3 and 12 months of follow-up, the patients completed the SF-36 questionnaire and an additional questionnaire to evaluate their specific living conditions and their current New York Heart Association (NYHA) classification.
The SF-36 is a self-administered instrument that takes about 15 minutes to complete. Originally developed as a multipurpose health survey instrument, the SF-36 has been translated in >50 countries as a part of the international QOL assessment project and has become the most extensively validated and generic instrument used for measuring QOL. The SF-36 consists of 36 items grouped in 8 general health parameters: physical functioning, role physical, bodily pain, general health, role emotional, social functioning, vitality, and mental health. The number of possible responses per item varies from 2 to 6. For each parameter, the scores are calculated and transformed to a scale from 0 to 100, with higher scores reflecting a better QOL. Each item measures functioning in different aspects of daily life ( Figure 1 ).

The 8 parameters could be summarized in 2 summarized scores: the physical component score and mental component score (MCS). The questionnaire is designed to take into account the status of QOL during the previous 4 weeks. Summary scores for the SF-36 were generated according to the scoring algorithms published by their developers ( Figure 1 ).
To assess the patients’ current living condition, they were asked about the degree of independency at home. To describe their current independence, they were asked to choose among 5 possible categories: (1) living completely independently alone or with their spouse; (2) living independently alone or with their spouse and receiving minor help for cleaning and shopping; (3) living alone or with their spouse and receiving major help for dressing and assistance with personal hygiene; (4) living in an assisted-living facility; or (5) living in a nursing home facility.
Additionally, patients were asked whether they would again decide in favor of TAVI. This question could be answered either yes or no.
The results are presented as the mean ± SD. The results of the SF-36 are depicted as the mean ± SEM. For the between- and within-group comparisons of the mean values of continuous variables, the 2-paired t test was used. For comparisons between dichotomous variables, Fisher’s exact test or chi-square test was used, as appropriate. One-way analysis of variance for categorical variables and Pearson’s correlation coefficient calculations as a measure of linear association between paired continuous variables were used to identify potential patient-related and nonpatient-, procedure-related factors predictive of the extent of postprocedural QOL change, including all baseline characteristics and postprocedural parameters. The individual QOL change was calculated by the difference in the physical component score and MCS scores between baseline and after 3 and 12 months, respectively. In general, a p value of <0.05 was considered statistically significant. All statistical analyses were performed using the SPSS, version 16, software (SPSS, Chicago, Illinois).
Results
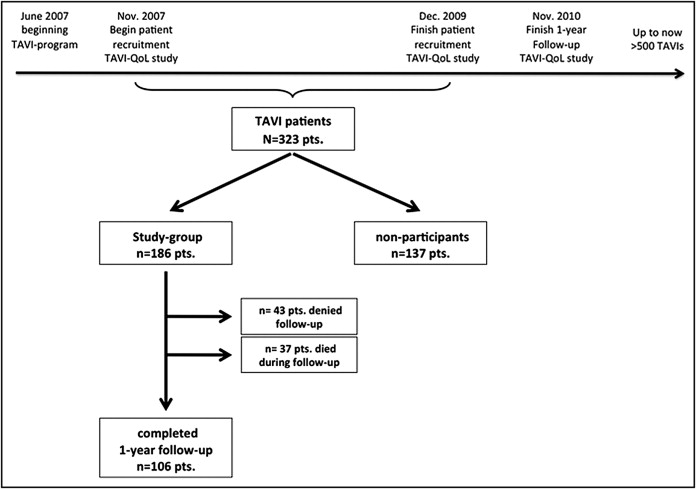
From November 2007 to December 2009, a total of 323 patients underwent TAVI at the German Heart Center (Munich, Germany). Of this population, 186 patients (118 women, mean age 81 ± 6.8 years) could be recruited for our prospective study. Of this group, 106 patients completed the 1-year follow-up. Figure 2 shows the follow-up data of the entire study population. The preoperative characteristics of the 186 recruited patients and those of the 137 nonrecruited patients are listed in Table 1 . These results show that both groups were comparable at baseline.
| Characteristic | QoL-group (n = 186) (mean ± SEM or n/%) | Non-participants (n = 137) (mean ± SEM or n/%) |
|---|---|---|
| Age | 80.8 ± 6.8 | 80.0 ± 7.2 |
| Female | 118/63 | 91/66 |
| Body mass index (kg/m 2 ) | 26.58 ± 4.7 | 26.45 ± 4.3 |
| Ejection fraction >50% | 116/62 | 82/60 |
| 35–50% | 40/22 | 32/23 |
| <35% | 30/16 | 23/17 |
| Effective orifice area (cm 2 ) | 0.68 ± 0.3 | 0.64 ± 0.2 |
| Δpmax (mmHg) | 78.8 ± 22.3 | 78.6 ± 26.5 |
| Δpmean (mmHg) | 48.4 ± 25.3 | 48.6 ± 17.5 |
| Mitral regurgitation >II | 40/22 | 29/21 |
| NYHA class at baseline | 3.07 ± 0.4 | 3.15 ± 0.3 |
| Previous cardiac surgery | 34/18 | 24/18 |
| Chronic kidney disease (Creatinine >1.5mg/dl) | 33/18 | 23/17 |
| Coronary artery disease | 69/37 | 50/37 |
| Pulmonary hypertension | 41/22 | 30/22 |
| Peripheral artery disease | 40/22* | 22/16* |
| Chronic obstructive pulmonary disease | 37/20 | 24/18 |
| Cerebrovascular disease | 27/15 | 17/12 |
| Log Euro-Score | 19.74 ± 12.1 | 20.41 ± 14.2 |
| STS-score | 6.5 ± 6.5 | 6.4 ± 4.4 |
The 30-day mortality rate was 10.2%, and the 1-year mortality rate was 20.6% in the study group. No significant difference was found in 1-year mortality between the study population and the nonparticipants (p = 0.1). The postprocedural characteristics of the study population and the nonparticipant group are listed in Table 2 .
| Characteristic | QOL Group | Nonparticipants |
|---|---|---|
| Transapical | 53 (28%) | 47 (34%) |
| Transarterial | 133 (72%) | 90 (66%) |
| Effective orifice area (cm 2 ) | 1.49 ± 0.4 | 1.51 ± 0.4 |
| Δpmax (mm Hg) | 21.7 ± 6.7 | 21.2 ± 6.6 |
| Δpmean (mm Hg) | 12.2 ± 3.9 | 11.9 ± 4.0 |
| Aortic valve regurgitation moderate or greater | 27 (14%) | 13 (10%) |
| Redo valve | ||
| Transcatheter | 3 (2%) | 1 (1%) |
| Surgical replacement | 4 (3%) | 2 (2%) |
| Pacemaker implantation | 32 (18%) | 26 (21%) |
| De novo hemodialysis | 13 (7%) | 14 (11%) |
| De novo stroke | 9 (5%) | 9 (7%) |
| Postprocedural length of stay (d) | 9.6 ± 6.1 | 9.9 ± 7.2 |
| 30-Day mortality | 19 (10.2%) | 15 (11.2%) |
| 1-Year mortality | 37 (20.6%) | 36 (29.1%) |
Postprocedural hemodynamic improvement could be confirmed by echocardiography at 1 year of follow-up. The effective orifice area increased from 0.68 ± 0.3 to 1.49 ± 0.4 (p <0.001), and the mean aortic valve gradient decreased from 48.4 ± 25.3 to 12.2 ± 3.9 (p <0.001) compared to the preoperative value.
The mean NYHA class improved significantly from a mean of 3.1 at baseline to 1.9 at 3 months and 2.0 at 1 year (p <0.001 for NYHA at baseline vs 3 months and 1 year; Figure 3 ) . Noteworthy, although not statistically significant, the NYHA functional class increased slightly between 3 months and 1 year after implantation, with a larger fraction of patients in NYHA class III at 1 year after TAVI (14.1% vs 25.8%).

A total of 106 patients completed the 1-year follow-up protocol. Significant improvements occurred from baseline to 1 year of follow-up in the SF-36 scores for physical functioning (34.6 ± 2.3 vs 45.6 ± 2.7; p <0.001), role physical (20 ± 3.0 vs 34.2 ± 4.4; p <0.001), bodily pain (59.9 ± 3 vs 70 ± 2.7; p <0.01), general health (47.3 ± 1.5 vs 55.2 ± 2.1, p <0.001), vitality (35.9 ± 2 vs 48.5 ± 2; p <0.001), and mental health (62.2 ± 2.2 vs 67.3 ± 1.8; p <0.05). No significant improvement could be detected for social functioning (75.4 ± 2.5 vs 76.5 ± 2.6; p = 0.79) or role emotional (61.1 ± 4.3 vs 66.5 ± 4.7; p = 0.29; Figure 4 ) . At 3 months and 1 year of follow-up, the physical component score increased significantly compared to baseline (31.8 ± 0.9 vs 37.8 ± 1.2 and 36.9 ± 1.1, respectively, both p <0.001). In contrast, no significant change was seen in the MCS from baseline to 3 months and from baseline to 1 year (48.6 ± 1.2 vs 47.9 ± 1.1 and 49.6 ± 1.2; p = 0.67 and p = 0.18, respectively; Figure 5 ) . The physical component score decreased slightly from 3 months to 1 year of follow-up (p <0.05).

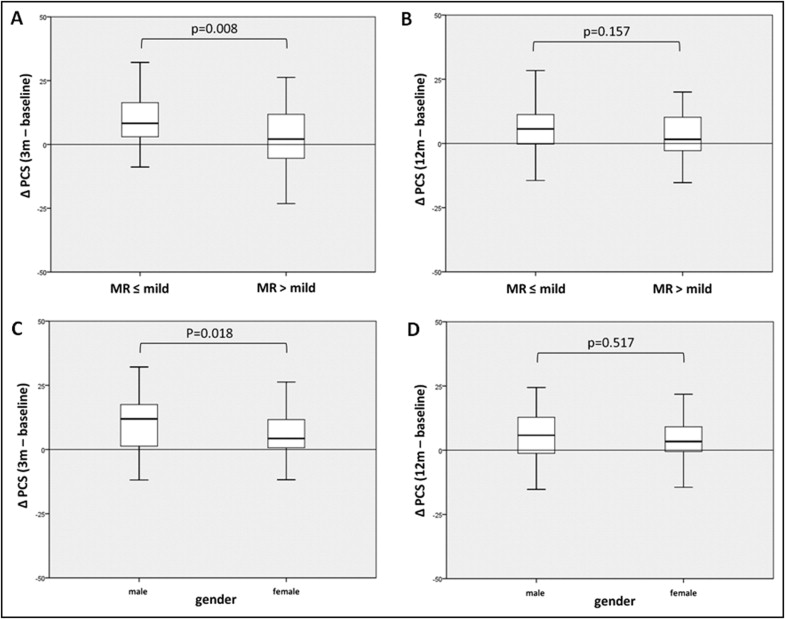
One-way analysis of variance and Pearson’s correlation coefficients analysis was used in an effort to identify potential patient-related and nonpatient-, procedure-related factors predictive of the degree of postprocedural QOL improvement after 3 and 12 months, respectively, compared to baseline. A degree of mitral valve regurgitation greater than mild was predictive of lower QOL improvements. At 3 months, the difference reached statistical significance. After 12 months, however, only a statistical trend could be documented ( Figure 6 ) . Likewise, female gender was associated with less improvement after 3 months. The difference failed to reach statistical significance after 12 months ( Figure 6 ). A significant minimal correlation was seen between the Society of Thoracic Surgeons score and the extent of QOL improvement after 3 months, and higher Society of Thoracic Surgeons scores were associated with lower QOL benefits ( Supplementary Figure 1 ). For the other factors listed, no significant associations with the degree of QOL change at 3 or 12 months were found: all baseline characteristics, including preoperative maximum/mean pressure gradient, effective orifice area, ejection fraction, preoperative NYHA class, height, weight, body mass index, co-morbidities (i.e., renal insufficiency, coronary artery disease, pulmonary hypertension, peripheral artery disease, chronic obstructive pulmonary disease, cerebrovascular disease), log European System for Cardiac Operative Risk Evaluation, type of valve implanted, presence of residual aortic regurgitation, patient–prosthesis mismatch, and procedural and postprocedural parameters, including procedure-related complications (stroke, procedure-related kidney injury, pacemaker implantation), postprocedural length of hospital stay, maximum/mean pressure gradients, and effective orifice area at 12 months (data not shown).
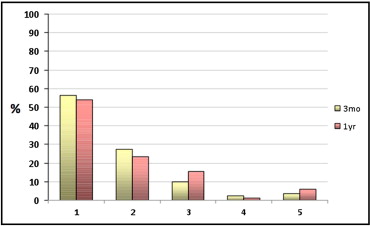
At 3 and 12 months after TAVI, 85% and 73% of our patients, respectively, were able to live independently or with only minor help at home ( Figure 7 ) . Although the number of patients who required major assistance at home (group 3) increased slightly, the overall difference from 3 months and 1 year did not reach statistical significance (p = 0.29). Most patients who underwent TAVI reaffirmed their decision to undergo TAVI at 3 and 12 months after the procedure (86.2% and 88.6% of the patients at 3 months and 1 year after TAVI, respectively).