Level of aortic injury
Direct signs
Indirect signs
Minimal aortic injury
Intraluminal thrombus: round or triangular intraluminal filling defect attached to the wall of the aorta Intimai flap: small (<1 cm), thin (linear) filling defect Intramural hematoma: High-attenuation material in the wall of the aorta, which may appear crescentic or circumferential
Mediastinal/periaortic hematoma
Contained rupture
Saccular pseudoaneurysm Fusiform pseudoaneurysm
Mediastinal/periaortic hematoma
Free rupture
Extravasation of contrast material
Mediastinal/periaortic hematoma Hemopericardium if injury involves the ascending aorta

Fig 1 a–c.
Minimal aortic injury. A linear filling defect, likely representing an intimal flap (arrows), is seen on axial computed tomography (CT) images (a) and on coronal reformats (b) in the descending thoracic aorta in a 38-year-old man who was involved in a motor vehicle accident. Three days after the accident, the intimal flap appears more rounded (c), possibly due to thrombus formation. On a follow-up CT prior to hospital discharge 3 weeks later, the intraluminal findings had resolved without intervention
Injuries that involve more than the intima are regarded as severe aortic injuries. In contained rupture, or aortic pseudoaneurysm, the tear involves both the intima and media, which bulge outwardly, held in place by the intact adventitia. Adventitial tears may involve 360° of the aortic wall, so that the pseudoaneurysm appears fusiform or barrel-shaped (Fig. 2). When the tear involves only a portion of the adventitia, the pseudoaneurysm bulges eccentrically from the aorta, typically in the region of the aortic isthmus.

Fig 2.
Contained aortic rupture. A fusiform pseudoaneurysm has formed in the proximal descending thoracic aorta. This occurs when the intima and media are torn and the pseudoaneurysm is contained by the intact adventitia
The stress placed on the aortic wall during sudden deceleration may result in complete rupture, with disruption of all three layers of the aortic wall — intima, media, and adventitia — with extravasation of blood into the adjacent anatomic compartment (Fig. 3). In some patients with complete rupture of the descending thoracic aorta, mediastinal tissues and the periaortic hematoma can produce a tamponade effect, preventing rapid exsanguination. This is in contrast to free rupture involving the ascending aorta, when blood can rapidly fill the pericardial sac, causing cardiac tamponade and death. It is important to recognize free rupture on imaging and to distinguish it from contained rupture. Although delayed repair may be considered in patients with aortic pseudoaneurysm, or contained rupture, immediate repair is necessary for patients with free aortic rupture.

Fig 3.
Free rupture. The extravasation of contrast medium from the transverse thoracic aorta is diagnostic of injury involving all three layers of the aortic wall. Mediastinal hematoma is also present, an indirect sign of aortic injury
In a patient with blunt trauma or deceleration injury, mediastinal hematoma is most commonly due to small venous injury and is therefore considered an indirect sign of aortic injury. Mediastinal hematoma associated with aortic injury is typically adjacent to the transverse and descending thoracic aorta and may dissect superiorly in the extrapleural space to form an “apical cap.” Mediastinal hematomas not in contact with the aorta but located in the anterior or posterior mediastinum are more likely to be related to chest wall or spinal fractures [6].
Cardiac Herniation
Cardiac herniation as a result of a traumatic tear of the pericardium is an uncommon occurrence but may be considered in the patient with fluctuating blood pressures after intravenous fluid administration together with tachycardia and dilated jugular veins [7]. Although cardiac-axis deviation may be apparent on a chest radiograph, more specific signs of cardiac herniation are better seen on CT and include the “empty pericardial sac,” as air fills the space remaining once the heart is displaced into the hemithorax, and the “collar sign,” resulting from the pericardium pinching the heart as it herniates through the pericardial tear. The tear is typically a longitudinal one located along the pericardiophrenic nerve and occurs more commonly on the left side. The mortality of patients with cardiac herniation is high, with death resulting from torsion along the inferior vena cava and great vessels and cardiac strangulation [8].
Hemopericardium
Hemopericardium should raise suspicion of injury to the heart, ascending aorta, or coronary arteries. It is most commonly associated with injury to the aortic root and ascending aorta but may also result from cardiac chamber rupture, myocardial contusion, and coronary artery laceration [8]. Simple fluid should demonstrate attenuation values of 0–10 Hounsfield units (HU) whereas hemopericardium will have attenuation values in the 35-HU range. The rapid accumulation of hemopericardium may result in cardiac tamponade. The latter diagnosis in patients with blunt chest trauma is suggested when CT demonstrates a triad of high-attenuation pericardial effusion, distention of the inferior vena cava and renal veins, and periportal low-attenuation fluid [8].
Esophageal Injury
Esophageal injuries caused by external, non-iatrogenic trauma are rare but potentially catastrophic. Mortality for undiagnosed rupture after 24 h is 10–40%. Chest radiographs may reveal pleural effusions, left sided if the lower third of the esophagus is injured, right sided if the upper two thirds is injured. Pneumomediastinum is also commonly seen but is nonspecific and usually not related to esophageal or tracheobronchial injury (see below): instead, it represents alveolar rupture and the dissection of air along bronchovascular sheaths to the mediastinum, the so-called Macklin effect (Fig. 4). Fluoroscopic esophagography is moderately sensitive (75%) for esophageal injury and very specific but it can be technically difficult to perform in critically ill patients. In a study of a small group of patients, CT esophagography performed after the ingestion or instillation of contrast and effervescent granules was very accurate in the detection of injury [9]. More recent studies following a similar protocol with the exception of the effervescent granules showed a high specificity but a sensitivity of only 50% [10].
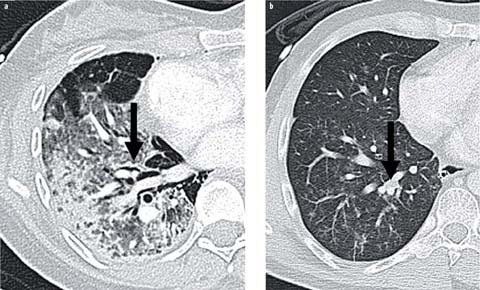
Fig 4 a, b.
Two patient with acute diffuse lung disease. a Acute respiratory distress syndrome (ARDS) with dependent consolidation and midlung ground glass opacities. The pneumomediastinum is due to the Macklin effect (arrow). b Trauma with acute aspiration causing tree in bud opacities and secretions in segmental bronchi (arrow)
Tracheobronchial Rupture
Tracheobronchial injury as a result of blunt-force trauma is uncommonly seen, as the majority of patients die before reaching the hospital. In a review of 88 surviving patients reported in the literature, the rupture involved the right main bronchus in 41 (47%), and 76% of the injuries were within 2 cm of the carina [11]. The median time until diagnosis was 9 days. Chest radiography may show indirect signs of tracheobronchial rupture, including cervical subcutaneous emphysema, pneumomediastinum, and persistent pneumothorax despite satisfactory positioning of a thoracotomy tube [12]. The “fallen lung sign” describes a collapsed lung lying in a dependent position, tethered to the hilum by pulmonary vessels (Fig. 5) [13]. Although originally described on chest radiography, this can also be seen on CT, which may demonstrate disruption in the wall of the trachea or bronchus; however, this is more readily identified at bronchoscopy, which should be performed in any patient with suspected tracheobronchial injury.
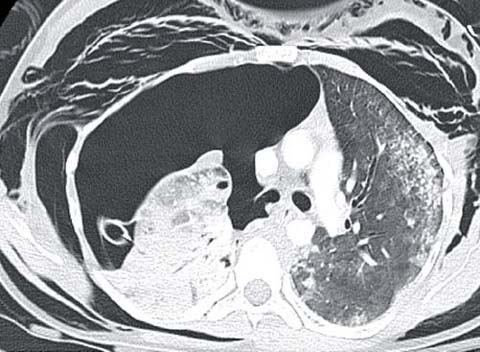
Fig 5.
Bronchial rupture. The lung lies in a dependent position within the right hemithorax, consistent with the “fallen lung sign.” Additional evidence of bronchial rupture in this case includes disruption of the bronchus, extensive subcutaneous emphysema, and a large pneumothorax despite satisfactory positioning of a thoracotomy tube
Pleural Space
Pneumothorax
Pneumothorax is second only to rib fractures in its prevalence among patients with blunt chest trauma. Rates vary widely from 5 to 64%, with a recent large series reporting an incidence of 16%. Some patients will develop tension pneumothorax, in which the pleural pressure rises sufficiently to impair venous return, causing hemodynamic instability. A chest radiographic finding of mediastinal shift is not specific for tension pneumothorax; rather, the diagnosis is made on clinical grounds.
Many trauma patients will receive only supine chest radiography, mandating a search for radiographic signs in addition to a pleural line, which may not be visible due to the predilection of pleural air to collect antero-inferiorly in supine patients. The “deep sulcus sign,” indicative of an abnormally deep and widened costophrenic sulcus, is the most commonly missed finding of a pneumothorax on supine radiographs. The presence of the “double diaphragm sign,” in which air outlines both the dome of the diaphragm and the anterior costophrenic sulcus (seen extending from the seventh costochondral cartilage medially to the 11th rib laterally), may increase the specificity but in general the sensitivity of supine radiographs in detecting pneumothorax remains <25% [14].
The limitations of chest radiography have stimulated the use of bedside ultrasound in the detection of pneumothoraces [15, 16]. In the absence of a pneumothorax, high-frequency probes readily demonstrate the to and fro sliding of the parietal and visceral pleura surfaces, the “sliding lung sign. “B lines”, caused by echo reverberations of the air-filled lung, appear as narrow hyperechoic ray-like opacities. While the presence of a sliding lung sign and B lines has a very high negative predictive value, multiple sites in the chest, and not only in the area of the ultrasound probe, must be evaluated. In well-trained hands, the sensitivity of ultrasound for pneumothorax is much greater than that of supine chest radiography, ranging between 50 and 95%.
CT remains the standard for the detection of pneumothoraces against which all other imaging is judged. However, the utility of detecting occult pneumothoraces, whether by CT or ultrasound is tempered by the more recent surgical literature showing that many of the small pneumothoraces not seen on radiographs have a benign course and may not routinely warrant tube thoracostomy drainage.
Hemothorax
Hemothorax occurs in 30–50% of blunt injuries but more commonly requires surgical intervention following penetrating trauma. On supine radiographs a posterior layering hemothorax can cause hazy opacity of the entire hemithorax through which the pulmonary vasculature is visible. Hemothorax is more easily detected when it is accompanied by a rim of fluid displacing the lung from the lateral and apical chest wall. Hemothorax is readily visible on CT, manifesting as pleural fluid (35–70 HU) and in some cases demonstrating a hematocrit sign in which the densest clot is seen in the dependent pleural space. High attenuation within 10–15 HU of vascular structures is indicative of active hemorrhage, usually arterial.
Following tube thoracostomy, pleural blood loss ⩾250 ml/h or greater >1000–1500 mL often indicates the need for thoracotomy [17, 18]. Initial CT imaging showing a layering hemothorax thicker than 24 mm is a relatively specific indicator that blood loss will exceed this threshold [18]. For patients who do not undergo initial thoracotomy and are instead treated with tube thoracostomy, CT is useful in detecting retained hemothorax. Most patients with a 500-mL retained hematoma require video-assisted thoracoscopy for its evacuation in order to prevent complications, principally empyema. Due to the typical presence of extensive associated parenchymal damage, chest radiography is neither sensitive nor specific for identifying a retained clot. In one series, half of the cases selected for surgical intervention by radiography showed no significant hematoma on chest CT [19].
Extrapleural Hematoma and Chylothorax
When the parietal pleura remains intact, blood may accumulate in the extrapleural space rather than within the pleural space. These extrapleural hematomas can be identified on CT by the inward displacement of extrapleural fat. They are not treated by tube thoracostomy (Fig. 6). Collections that are biconvex may represent an arterial bleeding source and are more likely to require surgical intervention [20].

Fig 6.
Extrapleural hematoma. Blood has accumulated in the extrapleural space following blunt force trauma to the left chest wall. Extrapleural fat is displaced inwardly (arrow). The biconvex shape and the high-attenuation material within the hematoma suggest an active arterial bleeding source, which may require embolization or surgical intervention
Chylothorax is an uncommon complication of chest trauma. It can result from penetrating trauma to the upper mediastinum that injures the thoracic duct as it ascends to the left of the esophagus, resulting in a left sided pleural effusion [21]. Blunt injury to the thoracic duct is often related to hyperextension of the spine and occurs most commonly at the level of the diaphragm, where the duct is located in the right hemithorax, thus giving rise to a right pleural effusion. Pleural fluid from a chylothorax may be lower in attenuation than water due to its fat content but in many cases co-existing protein in the fluid raises its attenuation to that of other pleural effusions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


