Test
Measured variables
Physiopathological diagnosis
Spirometry and flow/volume loop
Forced flows and volumes:
Expiratory: PEF, FVC, FEV0.5, FEV0.75, FEV1, FEV6, FEV1/FVC, FEF25, FEF50, FEF75, FEF25–50
Inspiratory: FIF50, FEF50/FIF50
Obstructive ventilatory alteration (with or without decreased FVC)
Restrictive ventilatory alteration
Bronchodilator response
Fixed central airway obstruction
Variable intra- or extrathoracic central airway obstruction
Measurement of static lung volumes:
Plethysmography
Nitrogen washout
Helium dilution
Volumes and capacities not measurable with spirometry: FRC, RV, TLC
Restrictive lung disease
Air trapping
Hyperinflation
Bronchial challenge test
Direct: methacholine, histamine
Indirect: exercise, mannitol, adenosine
PC20
or
Increased airway resistance
Presence and degree of bronchial hyperreactivity
Airway resistance
Plethysmography
Rint
IOS
Specific resistance and airway conductance
Airway resistance
Fres, Rrs5, Rrs20, Xrs5, Zrs, reactance area
Increase in airway resistance
Increase or decrease in compliance (IOS)
Bronchodilator response
Bronchial hyperreactivity
Diffusing capacity of the lung for carbon monoxide
DLCO
Alteration of the diffusing capacity of the alveolar–capillary membrane
Measurement of static pressures
MIP
MEP
Sniff nasal test
Cough PEF
Strength of inspiratory muscles
Strength of expiratory muscles
Ability to mobilize secretions
Maximal voluntary ventilation
Maximum amount of air inhaled and exhaled within 1 minute
Thoracopulmonary capacity
Resistance to fatigue, airway resistance, respiratory drive
6-Minute walk test
Distance traveled
Functional capacity to exercise
Cardiac capacity, respiratory capacity, muscular function capacity
Spirometry and the Flow/Volume Curve
Definitions of lung volumes, flows, and capacities
Tidal volume (TV) : volume of inspired and expired air during normal breathing |
Inspiratory reserve volume (IRV) : volume of air that enters the lungs when a deep inspiration is performed, above TV |
Expiratory reserve volume (ERV) : volume of air exhaled during a deep expiration after a normal expiration |
Residual volume (RV) : volume of air remaining in the lungs after a maximum expiration |
Vital capacity (VC): sum of the maximum expired volume after a maximal inspiration |
SVC: slow vital capacity |
FVC: forced vital capacity |
Inspiratory capacity (IC) : maximum amount of air that can be inspired after normal expiration |
Functional residual capacity (FRC) : volume of air that remains in the lungs after normal expiration |
Total lung capacity (TLC) : maximum volume of air that the lungs can contain |
RV/TLC ratio: percentage of RV in relation to TLC |
Forced expiratory volume in a given time (FEVt) : volume of air expired during the FVC maneuver from TLC in a given time (e.g., 0.5, 0.75, 1, or 6 seconds) |
FEV1/FVC ratio: percentage of exhaled volume in 1 second in relation to FVC |
Forced expiratory flow at 25–75% of FVC (FEF25–75) : slope of the spirometric volume/time curve between 25% and 75% of FVC |
Forced expiratory flow at 25%, 50%, or 75% of FVC (FEF25, FEF50, FEF75): forced expiratory flow when 25%, 50%, or 75% of FVC has been exhaled |
Forced inspiratory flow at 50% of forced vital capacity (FVC) (FIF50): forced inspiratory flow measured at the 50% point of the inspiratory part of the flow/volume curve |
Peak expiratory flow (PEF) : maximum flow velocity observed during the forced expiratory maneuver |
Spirometry is indicated to diagnose alterations in lung function in patients with respiratory symptoms and signs (pathologies that can directly or indirectly affect lung function) or with exposure to risk factors such as smoking, environmental contamination, radiotherapy, chemotherapy, or other drugs with known pulmonary toxicity. Spirometry is also indicated to assess anesthetic and surgical risks and the prognosis of patients with respiratory pathologies, to assess the response to different treatments (bronchodilators, inhaled corticosteroids, kinesiotherapy), and to control the advance of progressive pathologies such as neuromuscular diseases and cystic fibrosis.
The equipment used for spirometry should be calibrated daily.
The maneuver is performed with a maximum and rapid inspiration to reach the total pulmonary capacity, followed by a maximum expiratory effort 3–6 seconds in duration and/or a plateau of at least 1 second.
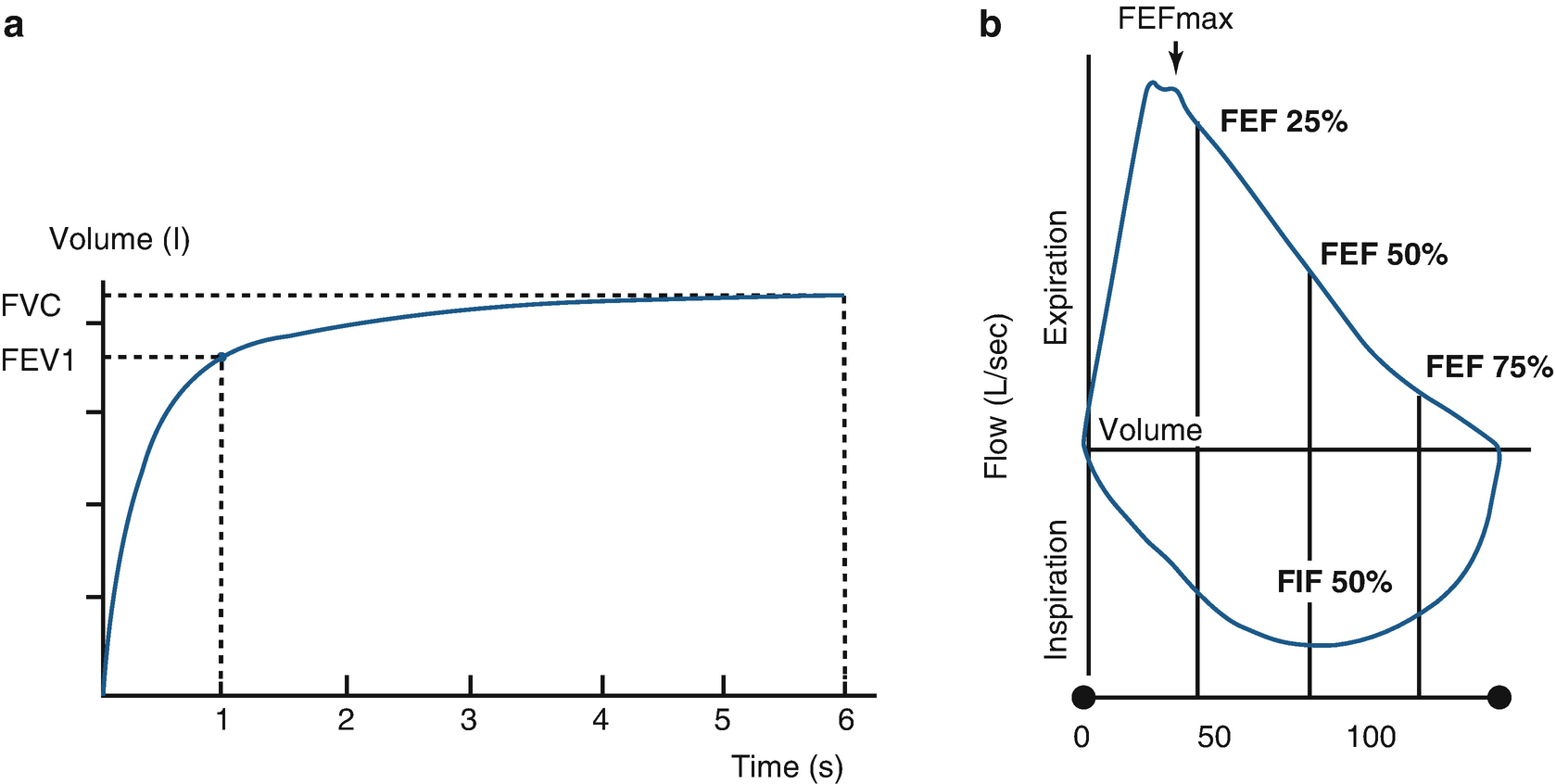
Spirometric curves. a Volume/time curve showing the forced expiratory volume in 1 second (FEV1) and in 6 seconds (FEV6). b Flow/volume loop showing the forced expiratory flow (FEF) at 25% (FEF25), 50% (FEF50), and 75% (FEF75) of the forced vital capacity (FVC), and the forced inspiratory flow (FIF) at 50% of the inspiratory loop. FEFmax maximum instantaneous flow achieved during a FVC maneuver
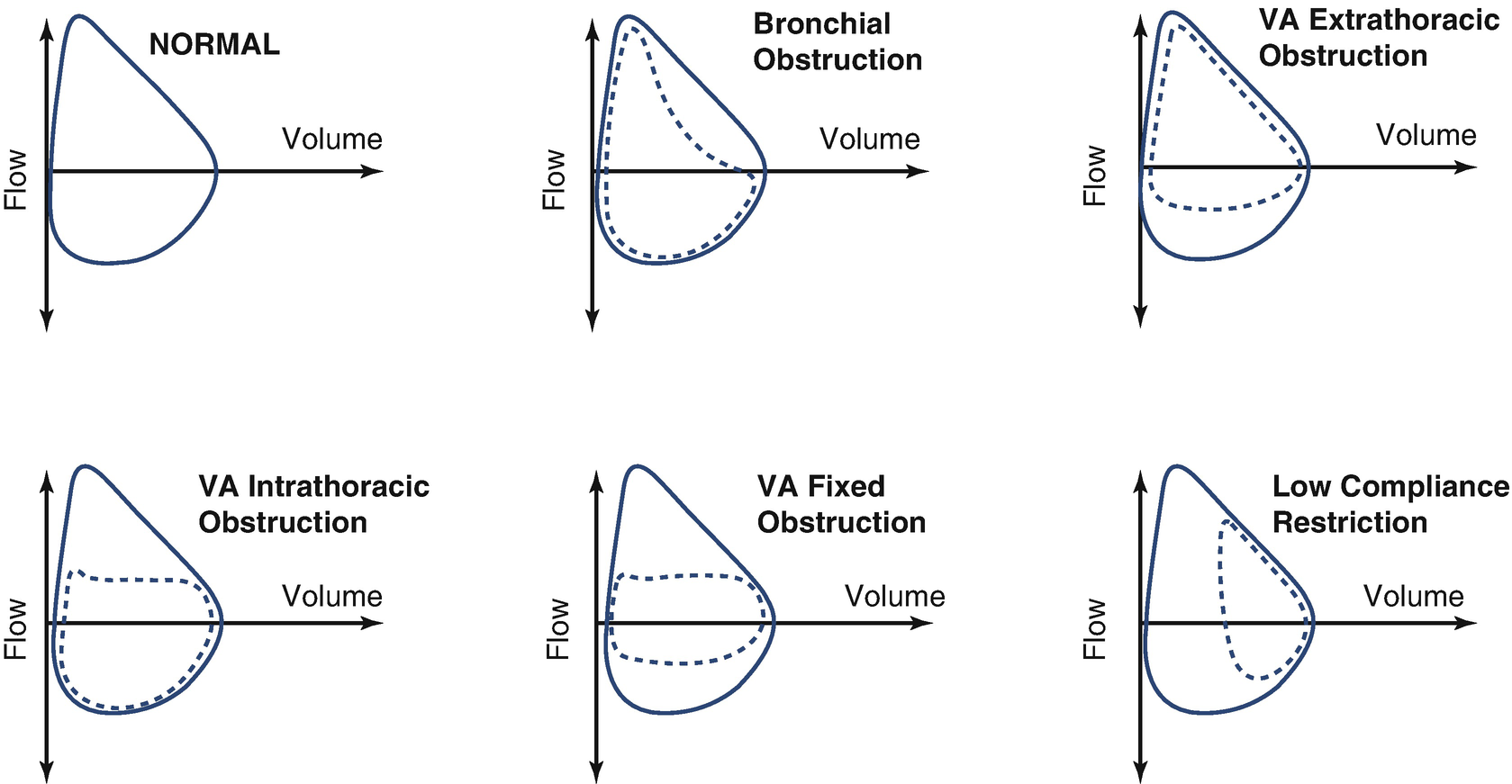
Alterations in the flow/volume loop: forms of the loop that display pathophysiological changes in the airway and lungs. Airway: Extrathoracic airway Obstruction; Intrathoracic airway Obstruction; Fixed airway obstruction
The spirometry test is repeated 15 minutes after administration of 400 μg of salbutamol in an aerosol form to assess the response to the bronchodilator. Any increase of 12% in FEV1 and/or 30% in FEF25–75 is considered a significant response (provided that the postbronchodilatory FVC does not vary more than 10% from the basal value).
The reference values that are used should be registered in the report. Those most widely used at present are Knudson, NHANES III (National Health and Nutrition Examination Survey III), and Gutierrez. The Global Lung Function Initiative (GLI) has recently developed reference equations that address an age range from 3 to 90 years, with differences according to the ethnicity of the population. A spirometry reading is considered normal when the values are above P5 or within ±1.64 standard deviations (Z score) of the reference values.
Types of alterations observed in spirometry
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


