Cystic fibrosis
Neonatal chronic lung disease
Postinfectious bronchiolitis obliterans
Recurrent bronchial obstruction that does not respond to the usual treatments
Central airway obstruction
Epidemiological and research studies
Measurement Conditions
Infants who are to be assessed through a functional respiratory study should fast for the previous 4 hours and be examined to rule out certain conditions in which the procedure is not advised, such as fever or the presence of secretions in the upper airway. The patient’s height and weight should be measured and the results should be compared with theoretical values. Prior to the procedure, 50–75 mg/kg of chloral hydrate is administered orally to induce a relaxed sleep, which in most cases lasts for 90–120 minutes. It is considered high-risk to administer this medication to patients with severe upper airway obstruction or those with some degree of hepatic, renal, or cardiac insufficiency.
The patient should be in a supine position during the study, with his or her head held straight in hyperextension. Small movements and flexing of the neck can alter the results and thus should be avoided. Arterial oxygen saturation and the heart rate are monitored continuously with an oximeter.
Methods
Measurement of Forced Expiratory Flow
Understandably, small children cannot perform maximum forced exhalations based on their total lung capacity for evaluation of the caliber of the peripheral airways. Different methods are used to prompt infants and small children to exhale forcibly. Deflation techniques, rapid thoracic compression at the tidal volume (RC-RTC), and rapid thoracoabdominal compression: RTC with preinsufflation are used to determine the magnitude of bronchial obstruction and variations in obstruction after administration of a bronchodilator or a bronchoconstrictor agent.
The deflation technique was the first to be developed, but it is no longer used, because it requires heavy sedation and intubation of the patient. Consequently, in this chapter, we discuss the other two methods.
Rapid Thoracoabdominal Compression Technique at Current Volume
Adler et al. (1978) and Taussig et al. (1982) described the rapid thoracoabdominal compression technique for determining the bronchial caliber in infants. It has been used to describe the normal growth and development of the airways in infancy, on the basis of which equations have been developed to establish the magnitude of bronchial obstruction, using a standard deviation score as a function of the sex and size of the subject. With this, the observed alterations in the functional response to the treatments applied in the respiratory clinic can be identified and evaluated.
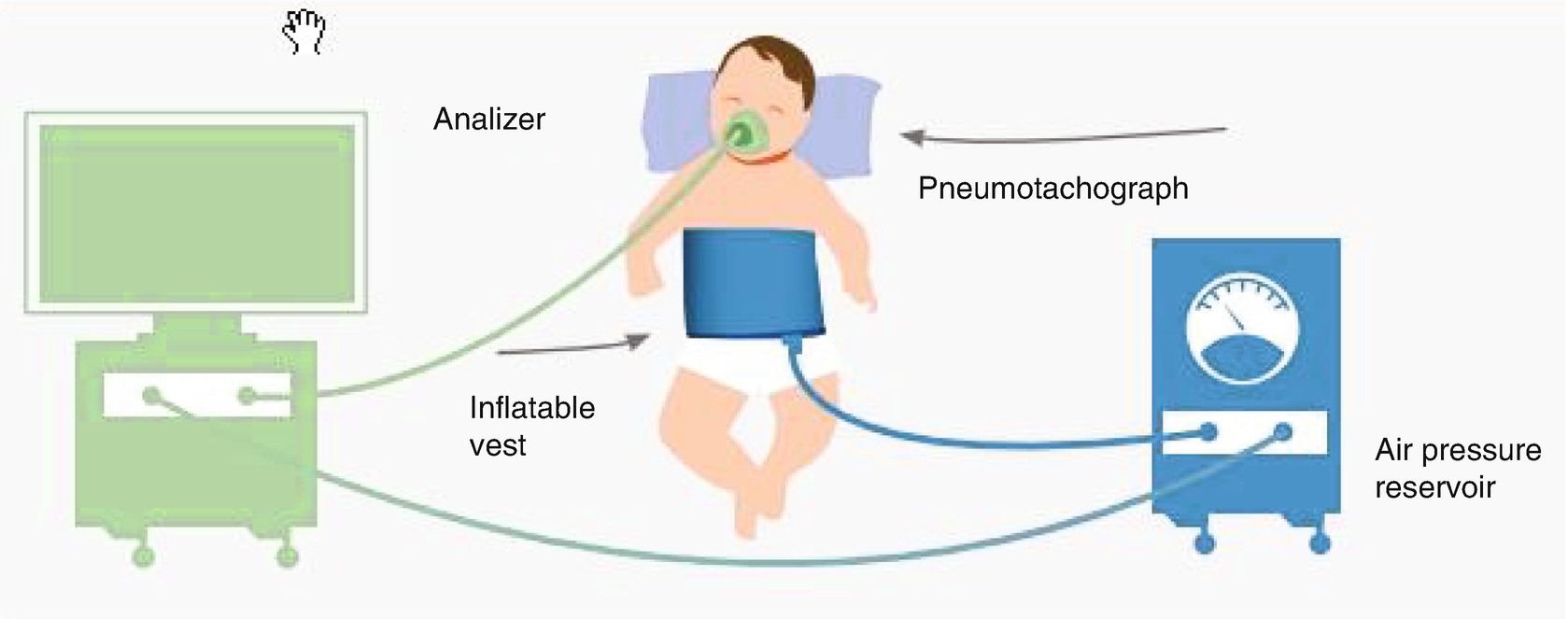
Equipment used for rapid thoracoabdominal compression at tidal volume (calculation of the maximum flow at the functional residual capacity (VmaxFRC))
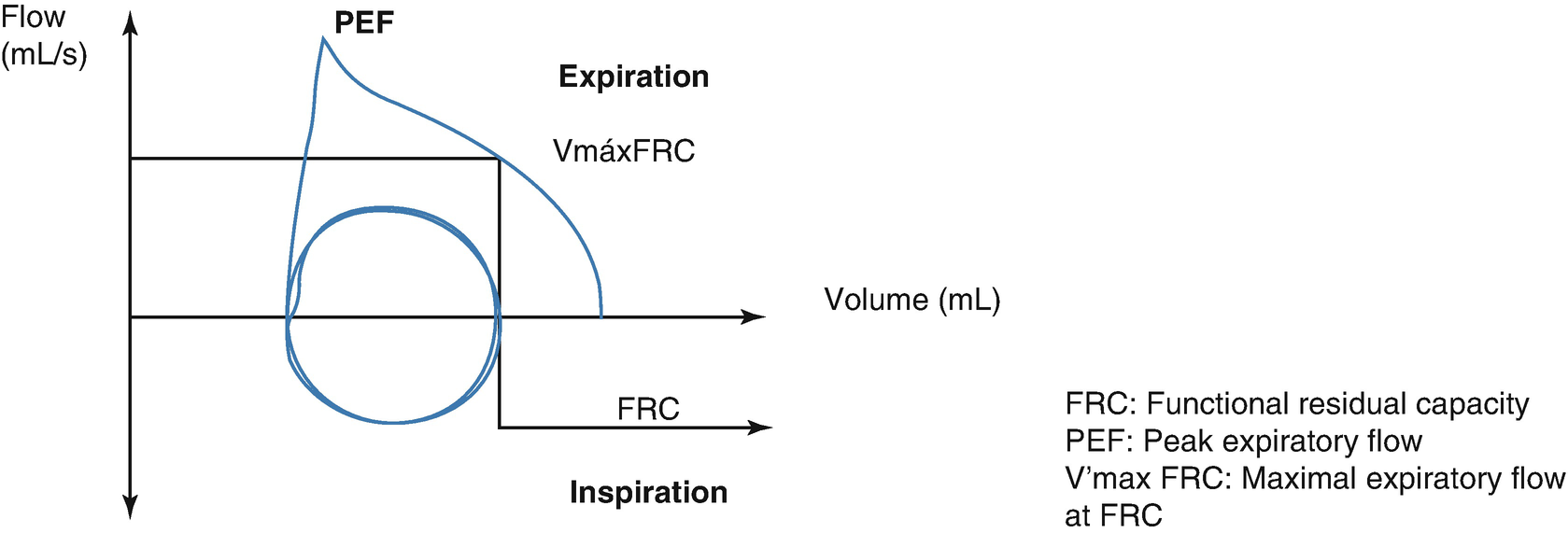
Partial forced flow/volume curve
While the highest pressures have no limit in relation to airflow in healthy infants, this is not the case in patients with bronchial obstruction, where much less pressure is required. Abrupt falls in airflow are attributed to glottic or pharyngeal closure, and they can be corrected according to the correct location in the neck. At least three acceptable and reproducible curves are obtained with maximum FRC values that do not vary by more than 10%, and VmaxFRC is the average of the three values. The curves obtained with this method are “partial,” given that they are based not on the total pulmonary capacity but, rather, on the end of the inspiration at the current volume.
Rapid Thoracoabdominal Compression Technique at a Volume with Previous Insufflation
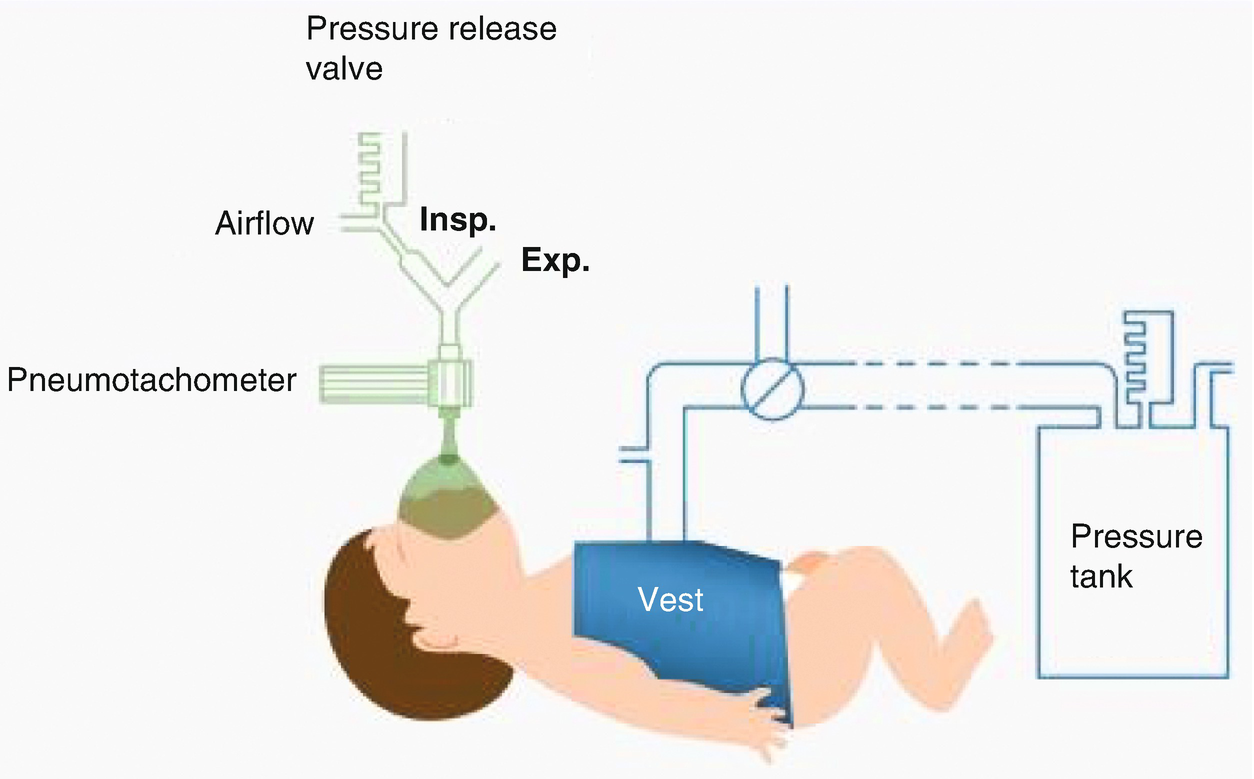
Rapid thoracoabdominal compression with previous insufflation
The insufflation system consists of an external source of air, valves to automatically occlude the airway or a Y connector for manual insufflation, and a safety valve to control the insufflation pressure. The jacket reaches maximum pressure in 70–100 milliseconds. Given that there is a small delay between insufflation and compression, it is a common practice to activate the compression 10–100 milliseconds before releasing the occlusion of the airway. One of the main discrepancies among users has been the application of different insufflation pressures to reach higher volumes. However, there is a consensus in the application of 30 cm of water pressure for older infants and 20 cm of water pressure for newborns and premature babies. The inspiratory flow is established at 1.5 times the current flow. The real pressure at the level of the mouth is monitored in real time so that the operator can adjust the flows and optimize the pressure being administered. There are also disparate criteria in the ventilation pattern before the forced expiration. The pulmonary insufflation rate depends on the lung volume and flow magnitude, while the volume reached for a standard pressure is directly proportional to the infant’s level of respiratory compliance. Most authors suggest 2–5 successive insufflations until pressure and volume plateaus are reached.
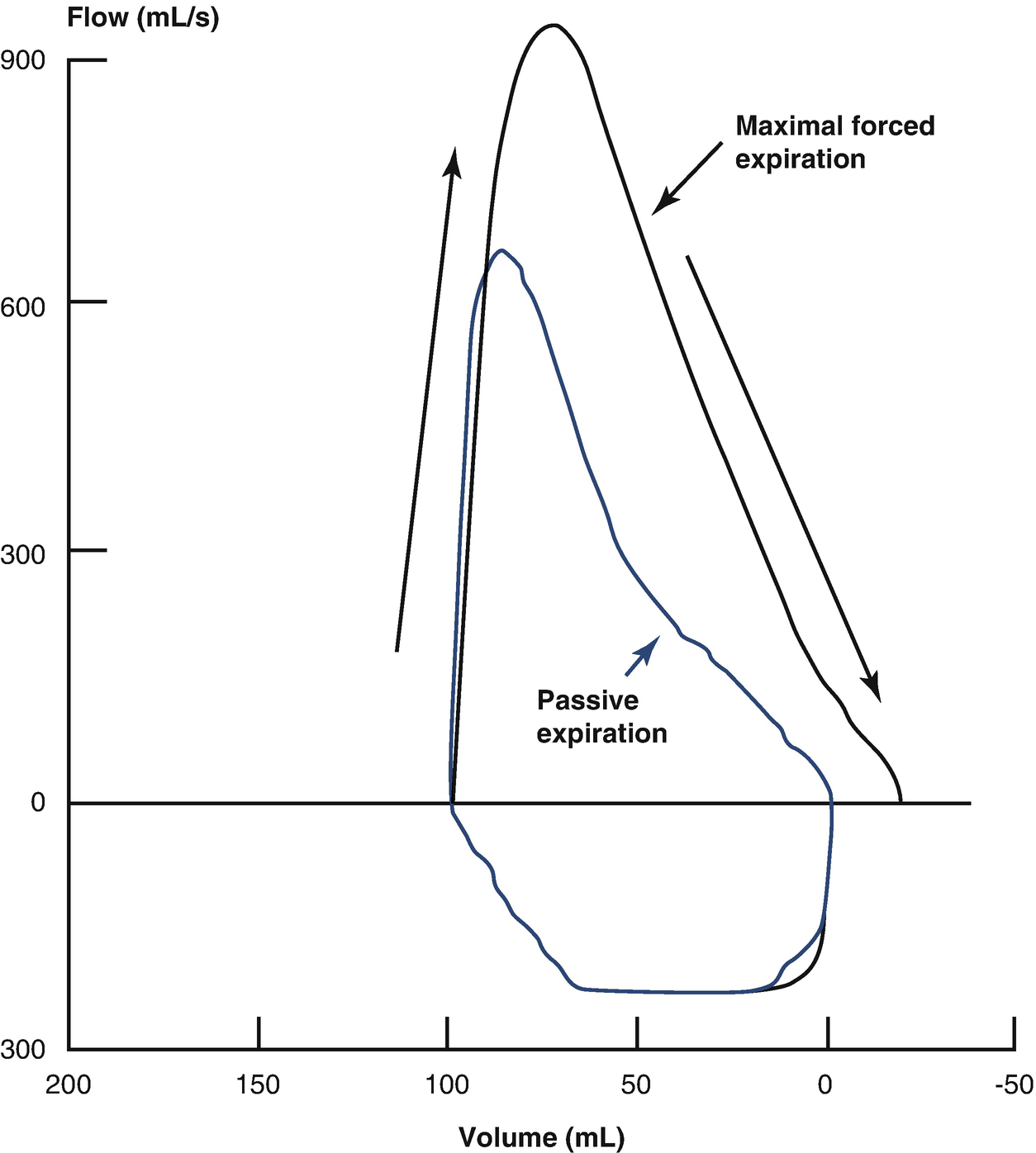
Maximum forced flow/volume (F-V) loop obtained by rapid thoracoabdominal compression with previous insufflation
Analysis of Breathing at Current Volume
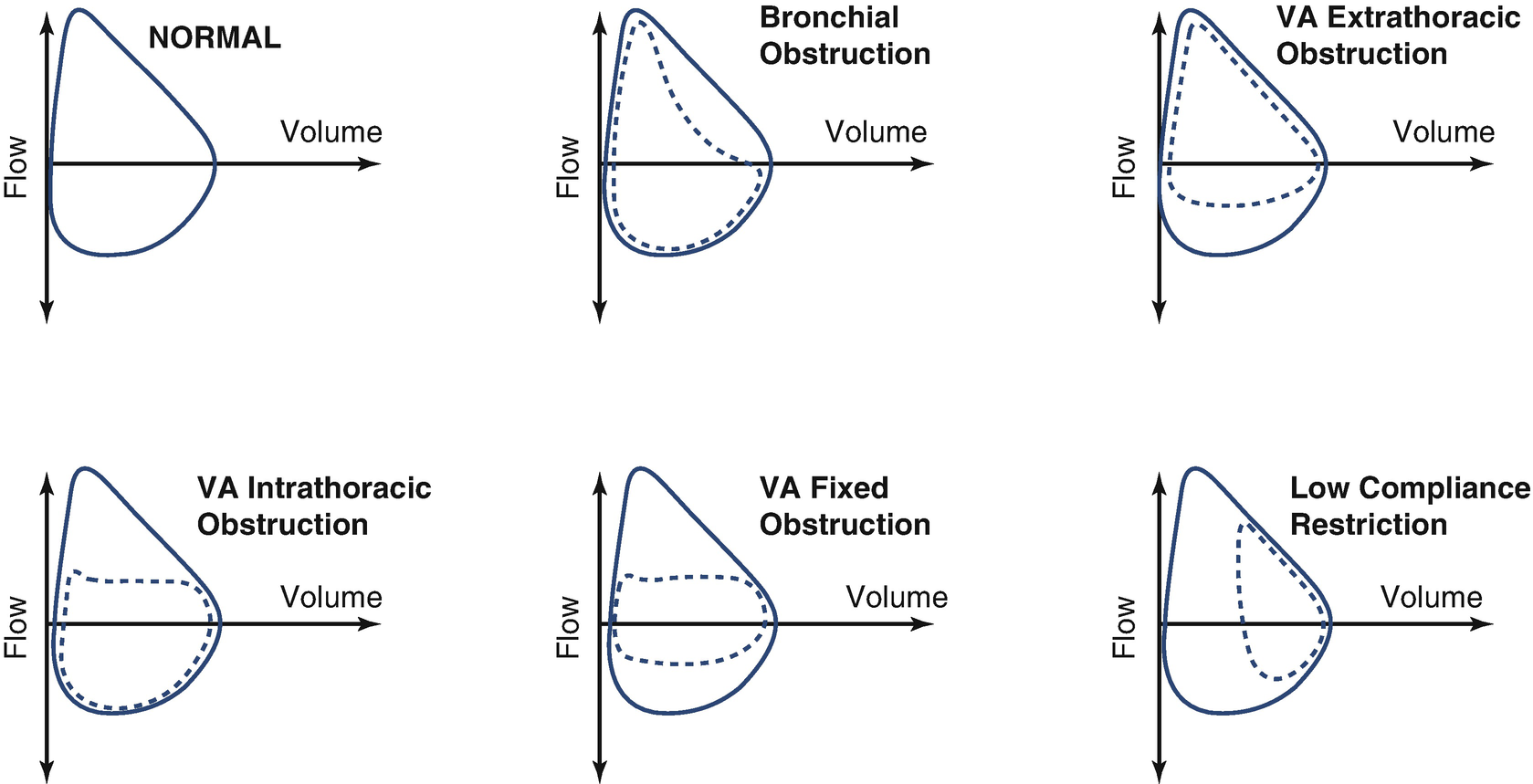
Flow/volume loop patterns
- (a)
Parameters that are altered in pulmonary elastic retraction disorders: the rate between the peak expiratory flow and current volume (PEF/Vc)
- (b)
Parameters that vary with obstructive pathologies: the percentages of volume and time to reach PEF

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


