Chapter 123
Occupational Vascular Problems
Mark K. Eskandari, Hari R. Kumar
Upper extremity work-related injuries are a major societal problem in regard to disability, cost, and loss of workdays. Occupational injuries affecting the shoulders, arms, and hands have been recognized for nearly 300 years and are generally categorized into injuries caused by accidents or injuries resulting from long-standing repetitive tasks.1 Injuries in the latter category are due to small but additive amounts of tissue damage sustained from repetitive motions; they are known collectively as cumulative trauma disorders. According to 2011 data released by the U.S. Bureau of Labor Statistics, injuries sustained from repetitive motion often result in longer duration of time away from work compared with other classes of injury.2 Although most of these injuries affect the musculoskeletal system, injuries to arteries and veins are known to occur.3 Work-related vascular injuries develop from excessive or exaggerated activity involving the shoulders, arms, or hands. Box 123-1 lists arterial disorders associated with occupational trauma.
Manual Labor Injuries
Hand-Arm Vibration Syndrome
The first cases of this injury were reported by Loriga in 1911 among Italian miners presenting with “dead finger.”4 Hamilton in 1918 made the connection between cold-induced blanching and numbness of the hands and use of pneumatic drills by stonecutters in Indiana.5 Subsequent work by Taylor and Pelmear6 and Ashe et al7 firmly established hand-arm vibration syndrome (HAVS) as a discrete clinical entity.
The disease has been referenced by many names, from the original dead finger to Raynaud’s of occupational origin, traumatic vasospastic disease, and vibration-induced white finger. The current designation of HAVS was introduced to reflect that the extent of involvement is more of the upper extremity than just the digit. Regardless of the name, the common initial symptoms are those of Raynaud’s phenomenon secondary to prolonged use of vibrating mechanical tools.
Clinical Findings and Risk Factors
The Taylor and Pelmear staging system is presented in Table 123-1.6 In the early stages, vibration injury may be manifested as slight tingling and numbness. Later, the tips of one or more fingers experience attacks of blanching, usually precipitated by cold. With continued progression, the affected area increases in size, and the blanching extends to the entire finger. Attacks of white finger typically last about 1 hour and terminate with reactive hyperemia (red flush) and often considerable pain. Prolonged exposure may induce bluish black cyanosis in the affected fingers. Only about 1% of cases progress to ulceration or gangrene.8
Table 123-1
Stages of Hand Arm Vibration Syndrome
| Stage | Condition of Digits | Work and Social Interference |
| 0 | Vibration exposure but no signs or symptoms | No complaints |
| 0T | Intermittent tingling | No interference with activities |
| 0N | Intermittent numbness | No interference with activities |
| 1 | Blanching of one or more fingertips, with or without tingling and numbness | No interference with activities |
| 2 | Blanching of one or more fingers with numbness, usually in winter | Slight interference with home and social activities; no interference with work |
| 3 | Extensive blanching; frequent episodes in summer and winter | Definite interference at work, at home, and with social activities; restriction of hobbies |
| 4 | Same as stage 3: extensive blanching, most fingers involved, frequent episodes in summer and winter | Same as stage 3, but occupation changed to avoid further vibration exposure because of the severity of signs and symptoms |
Updated from Taylor W, et al, editors: Vibration white finger in industry, New York, 1975, Academic Press.
Vibrating handheld machines (e.g., pneumatic hammers and drills, grinders, chain saws) have been implicated in HAVS. Such injury potential is not restricted to a few types of tools but applies to a variety of situations in which workers’ hands are subjected to transmission of vibration energy.9 There appears to be a linear relationship between the acceleration exposure dose (amount of acceleration and years of exposure) and the onset and severity of HAVS.10
The exact mechanism of injury is unknown. The frequency and intensity of vibration affect the extent of damage to the endothelium.11 Local platelet adhesion seems to be an important factor in arterial occlusion. It has been shown that sympathetic hyperactivity, in combination with local factors such as vibration-induced hyperresponsiveness of the digital vessels to cold, may be responsible for the finger-blanching attacks.12 In those with exposure to vibration injury, appearance of symptoms has also been correlated to smoking status.13
Diagnosis
Key features in the history include use of vibrating tools and symptoms of Raynaud’s phenomenon. For a vasospastic condition, the most promising single objective test is cold provocation and recording of the time until digital temperature recovers (see Chapter 15). Digital artery occlusion is best detected by recording the systolic pressure of the affected fingers with transcutaneous Doppler ultrasound14–16 or duplex scanning.17 In advanced disease, arteriography is helpful. Barker et al18 documented arterial occlusion by brachial arteriography in workers who complained of hand blanching and attacks of numbness. Other authors have reported on the use of arteriography in this injury.19–21
Arteriographic changes in HAVS can include multiple segmental occlusions of the digits and a corkscrew configuration of vessels in the hands.21 The extent of digital artery occlusion appears dependent on the frequency and duration of exposure.22
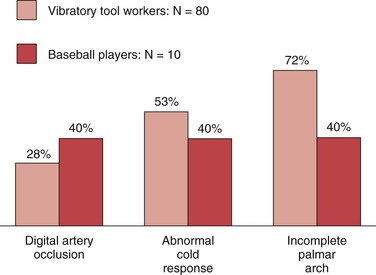
Of 80 workers (chippers) with HAVS investigated at the Blood Flow Laboratory at Northwestern University, 25 (31%) exhibited a significant reduction in systolic pressure in one or more digits.23 In 6 of the 25 workers, arteriography showed digital artery occlusion (Fig. 123-1). Incompleteness of the palmar arch was seen not only in the symptomatic hand but also in the contralateral, asymptomatic one. Raynaud’s phenomenon was present in 73 of 80 workers (91%). Abnormal cold response was observed in 53% of these workers (Fig. 123-2).

Figure 123-1 Arteriogram of the hand in a vibratory tool worker. Occlusion of the digital arteries (arrow) is apparent.
Treatment and Prevention
With onset of neurovascular symptoms that interfere with social or work activities, the initial treatment is discontinuation of use of vibratory tools.10 In advanced cases, a calcium channel blocker such as nifedipine (30 to 80 mg daily) may be useful. Calcium antagonists inhibit the response of arterial smooth muscle to norepinephrine and have been reported to be effective.24 Intravenous infusion of a prostanoid (prostaglandin E1, prostacyclin, or iloprost) is usually reserved for patients with digital gangrene.25 Surgical treatment, such as cervical sympathectomy or digital sympathectomy, is rarely needed.
Prevention is likely to be more effective than treatment. Personal protective equipment, such as gloves that limit exposure to cold and dampen transmission of vibration, should be used. Standards that limit the dose and duration of exposure to vibration have been set in place for factories and workplaces in the United States and internationally.10
Hypothenar Hammer Syndrome
Etiology and Incidence
The anatomy of the ulnar artery at the hypothenar eminence makes it vulnerable to injury with repetitive use of the palm of the hand in activities that involve pushing, pounding, or twisting. The ulnar artery and nerve travel in a tunnel known as Guyon’s canal that is bound by the pisiform and hamate bones. In this region, the ulnar artery is superficial and covered only by skin, subcutaneous tissue, and the palmaris brevis muscle (Fig. 123-3). Use of the palm as a hammer compresses the artery against the hook of the hamate bone, which acts as an anvil.
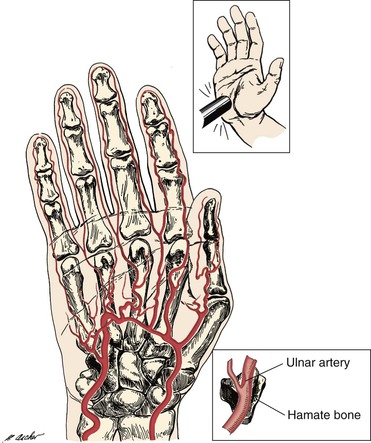
Figure 123-3 Mechanism of ulnar artery injury (upper inset) in a patient with hypothenar hammer syndrome. The terminal branch of the ulnar artery is vulnerable to injury because of its proximity to the hamate bone (lower inset).
Von Rosen (1934)26 and Guttani (1772)27 published the original reports of the disease, but it was Conn et al28 who first recognized the anatomic mechanism of injury and coined the term hypothenar hammer syndrome. Mechanics, factory workers, carpenters, masons, and any laborers who habitually use their hands as a hammer are at risk for the disease.29–31
The incidence of this rare entity is not precisely known as it is likely underrecognized. In Little and Ferguson’s study of 79 mechanics, 14% had evidence of ulnar artery occlusion but none had symptoms severe enough to seek medical attention.29 Studies focusing on cases of hypothenar hammer syndrome among referrals to tertiary centers for hand ischemia have found an incidence of 1.1% to 1.6%.31,32
The type of arterial abnormality observed often depends on the nature of the vessel injury but includes thrombotic occlusion, aneurysm formation, or both. Vasospasm and damage to the intima can result in platelet aggregation and thrombus formation.33 Damage to the media can lead to aneurysmal degeneration of the artery (Fig. 123-4), although this occurs less frequently. Thrombus formation can also occur within the aneurysm itself and lead to distal embolization.

Figure 123-4 Arteriogram of the hand of a carpenter. Note the aneurysm of the ulnar artery (arrow) caused by repetitive trauma from using the hand as a hammer.
Research by Ferris et al32 demonstrated that, in addition to vascular damage from repetitive trauma, underlying vessel abnormalities may also be responsible. Histologic examination of 19 resected ulnar arteries showed hyperplastic proliferation of the intima or media and disruption of the internal elastic lamina suggestive of fibromuscular dysplasia. In 13 patients for whom bilateral angiograms were available, 12 of 13 (92%) showed an abnormality in the contralateral asymptomatic ulnar artery. On the basis of this evidence, they proposed that the etiology of hypothenar hammer syndrome depends on the presence of underlying ulnar artery fibromuscular dysplasia with superimposed repetitive palmar trauma.
Clinical Findings and Diagnosis
Patients typically present with Raynaud’s phenomenon. However, several key features distinguish hypothenar hammer syndrome from similar syndromes.33 There is a preponderance of male smokers with a concomitant history of repetitive trauma to the hand.31 The distribution is asymmetrical, often involving only the dominant upper extremity. The cyanosis and pallor phases can occur, but the hyperemic redness is usually lacking.30 The digits affected tend to be the ulnar three fingers, with a distinct lack of involvement of the thumb.30,32
Physical examination may reveal cool or mottled digits; severe cases present with ischemic ulcers. A callus may be present over the hypothenar eminence. The result of Allen’s test is often positive, indicating ulnar artery occlusion. On occasion, an aneurysm is observed as a pulsatile mass in the hypothenar eminence.
Noninvasive imaging studies such as duplex ultrasound and contrast-enhanced computed tomography or magnetic resonance imaging have been used to make the diagnosis of hypothenar hammer syndrome.34–36 However, the “gold standard” imaging modality in hypothenar hammer syndrome remains invasive arteriography. Arteriography is extremely useful in diagnosis and planning of surgical treatment as it defines the type of vascular lesion (spasm, aneurysm, occlusion), shows the site and extent, and identifies the anatomy of the palmar arch and significant collateral vessels. A corkscrew pattern is typically observed in affected vessels.32 Regardless of which imaging modality is used, proximal arterial segments should be included in the examination to rule out upstream sources of embolization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree