Nonneoplastic Diseases of the Pleura
Allen P. Burke, M.D.
Marie-Christine Aubry, M.D.
Infections of the Pleura
Bacterial Infection and Empyema
Definition
Clinically, empyema is defined by the presence of microorganisms in pleural fluid, Gram stain, or culture; pleural pH < 7.2 associated with radiographic features of empyema; or frank pus in the pleural space at the time of thoracoscopy.1 The pathologic definition is that of purulent inflammation within the pleural cavity.
Etiology and Stages
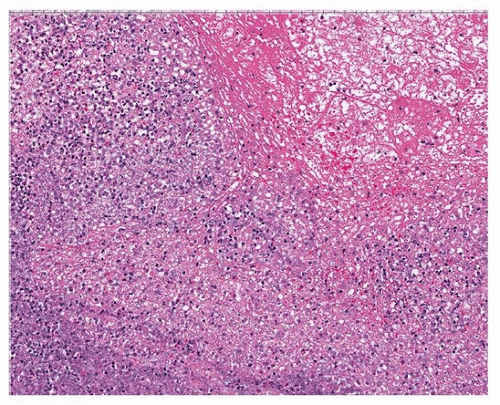
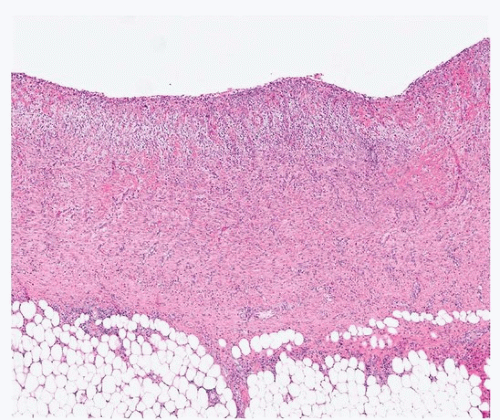
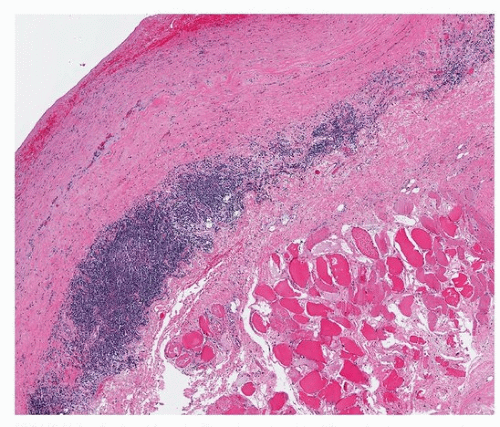
Empyema is caused by infected parapneumonic effusions, which begin as sterile fluid collections. The first phase is the exudative phase, with free-flowing, nonviscous fluid, which overlaps with parapneumonic effusion; the second is the fibrinopurulent phase (Fig. 95.1), with viscous fluid, loculations, and pleural peels; and finally there is the organizing phase, with fibrosis (Figs. 95.2 and 95.3).2 The causative organism or organisms are generally that of the adjacent pneumonia and reflect the clinical setting (Chapter 38).
Incidence
Pneumonias that result in either effusions or empyema occur in about 1 in 1,000 children.6 Community-acquired pneumonia in adults is complicated by empyema in 0.7% of patients.1 Patients who are immunocompromised are at increased risk for empyema following pneumonia.7,8,9
Organisms
Most commonly, an empyema develops from similar pathogens that cause a pneumonia.2 In community-acquired pneumonias, streptococci are the most frequent causes of pneumonia and empyema, with a propensity for pneumonias caused by Streptococcus viridans group. Less common organisms include Staphylococcus aureus, Pseudomonas aeruginosa, Haemophilus influenzae, and Mycoplasma pneumoniae.7,10,11 In immunocompromised patients, the bacterial etiology can be quite diverse and includes more frequent Gramnegative rods.9
Bacteria are isolated from blood, sputum, or pleural fluid. Because many pleural samples are culture negative, molecular studies are useful in determining the organism and species and serotype of streptococcus.10
Spontaneous Bacterial Empyema
Spontaneous bacterial empyema denotes bacterial infection of a previously sterile pleural effusion, in the absence of contiguous pneumonia. It usually occurs in patients with cirrhosis, at a rate of 1% to 2%.12
Prognosis and Treatment
The in-hospital mortality rate for patients with empyema is 4% to 15%.1
Approximately 40% of patients require surgical intervention, in the form of pleural decortication, obliteration of the pleural space with muscle flaps or omentum flaps, or by thoracoplasty.13 If only a chest tube is placed, tissue is generally not sampled, but fluid is obtained for microbiologic and cytologic analysis.6
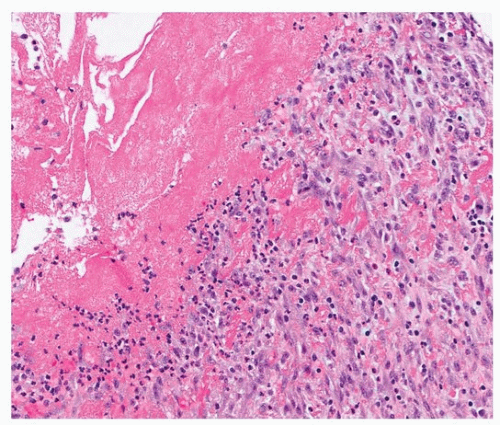 FIGURE 95.2 ▲ Empyema, organizing stage, pleural decortication. There is granulation tissue with abundant fibrin. |
Gross Findings
Grossly, empyema cavities are generally seen at autopsy at relatively advanced stages and consist of loculated masses with hemorrhagic fluid and frank pus that are generally within the pleural cavity. There may be adjacent abscesses within the lung parenchyma.
Microscopic Findings
Histologically, the findings that are seen in pleural decortications or pleural “peels” include fibrinous pleuritis, acute and chronic inflammation, and granulation tissue. In later stages, there is pleural fibrosis (Fig. 95.4). Occasionally, there is reactive mesothelial hyperplasia that rarely raises the concern for malignancy.
Fungal Pleural Infections
Fungal empyema is rare in community-acquired pneumonia.1 Candida is the most frequent species isolated, typically in mixed bacterial infections, and may be seen in spread from adjacent osteomyelitis, abscesses, or fistulas.2,3,5
Mycobacterial Infections and Empyema Necessitatis
Chronic cavitary tuberculosis frequently involves the pleural cavity. Empyema necessitatis is a rare form of empyema in which the pleural infection spreads outside of the pleural space into soft tissues of the chest wall and is usually caused by Mycobacterium tuberculosis. Computerized tomographic imaging will reveal a loculated fluid collection extending beyond the thoracic cage to involve the chest wall8 Rarely, Actinomyces israelii, streptococcus, Mucor, and staphylococcus pneumonia can cause empyema necessitatis.8,14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree