Echocardiography has emerged as the primary diagnostic tool for detecting cardiogenic and proximal aortic sources of peripheral arterial emboli. Two forms of echocardiograms are available: transthoracic (TTE) and transesophageal (TEE). The standard TTE has a diagnostic yield of 10% to 25% for identifying cardiac emboli in patients because it cannot visualize all heart chambers. It does evaluate the left ventricle more completely than a TEE, but it does not image the left atrial appendage, which is the most common site of thrombus in patients with atrial fibrillation. TTE is also limited by body habitus, young age, the presence of prosthetic heart valves, and overinflation of the lung as occurs in chronic obstructive pulmonary disease. Nevertheless, TEE can pick up greater than 50% of sources of cardiac emboli in patients with no clinically apparent heart disease.
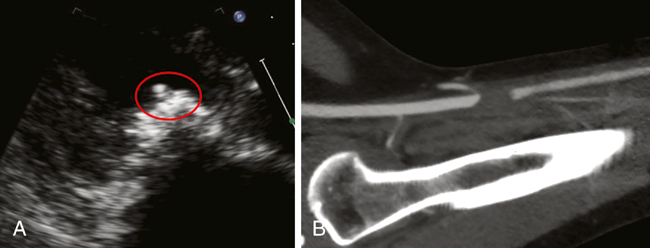
TTE is a useful first-line screening test because it can easily be done at the bedside without sedating the patient, as is required for TEE. TTE can detect most cardiac anomalies that predispose to arterial embolism (Figure 1), including prosthetic valves, vegetations, left ventricular aneurysms, dilated cardiomyopathy, mitral valve prolapse, and left ventricular thrombus. It also can evaluate for left ventricular dysfunction as well as delayed left atrial appendage emptying, both being risk factors for systemic emboli in patients with atrial fibrillation. Atrial septal defects can also be seen on TTE. Primary cardiac tumors, the majority of which are myxomas and sarcomas, can also be detected on TTE.
TEE evaluates the entire heart from the esophagus behind the left atrium. The left atrial appendage may be the source of thrombus in up to 40% of patients with valvular heart disease and peripheral emboli. In addition, TEE is highly sensitive in recognizing a patent foramen ovale and valvular strands and vegetations, especially in a patient with high clinical suspicion of infective endocarditis and a negative TTE. TEE is also a great adjunct to guide therapy for patients in atrial fibrillation in terms of short-term anticoagulation and subsequent cardioversion.
TEE carries the distinct advantage of being able to image the thoracic aorta and aortic arch. Complex aortic atheromas in the descending thoracic aorta can be evaluated, and the dynamic nature of TTE is sometimes better at identifying the embolizing aortic thrombi and mobile thrombus compared to the static contrast imaging of computed tomography (CT) or magnetic resonance imaging (MRI). A grading system is used to classify aortic atherosclerosis from lowest to highest embolic potential: grade I: normal or intimal thickening less than 4 mm; grade II: diffuse intimal thickening 4 mm or more; grade III: atheroma less than 5 mm; grade IV: atheromas greater than 5 mm; and grade V: any mobile atheroma.
The use of intravenously injected agitated saline for a bubble study can detect a right-to-left shunt by both TTE and TEE. Direct visualization of bubbles passing from the right atrium into the left atrium within three beats, either spontaneously or after valsalva maneuver, is diagnostic of a patent foramen ovale. Late appearance of bubbles may be a result of passage through lungs and then entry into the left atrium. The bubble load can define the size of the defect.