Noninvasive Diagnostic Testing
The Electrocardiogram
The 12-lead electrocardiogram (ECG) provides an enormous amount of useful information for the prediction of arrhythmia risk.
QRS Interval
Prolongation in the QRS interval with an intraventricular conduction delay (IVCD) or left bundle branch block (LBBB) pattern has consistently been correlated with an increase in total and arrhythmic mortality in patients with underlying cardiomyopathy. Right bundle branch block (RBBB) does not appear to be associated with a worse prognosis.
QT Interval
The QT interval is the ECG representation of cardiac repolarization. Prolongation in the QT interval in association with the development of polymorphic ventricular tachycardia is called torsades de pointes (TDP). QT prolongation with TDP can be a congenital abnormality or can be acquired.
Measurement of the QT Interval
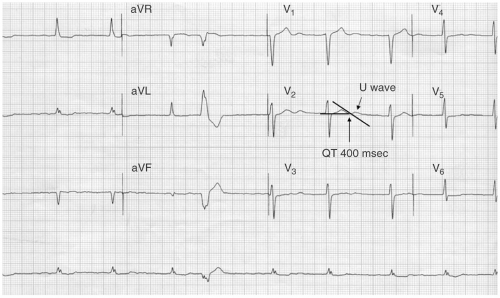
The QT interval is measured from the onset of the Q wave to the termination of the T wave. The end of the T wave is defined as the point at which the T wave crosses the baseline. If the baseline is difficult to assess, a line can be drawn from the preceding TP interval to the next TP interval. The lead with the most distinct T wave and clear termination should be chosen. Lead II or V2 are the most commonly utilized leads.
The U wave is a small positive or negative deflection which follows the QT interval (see Fig. 17-1). It is generally not included in the measurement of the QT interval unless it is >50% of the T-wave amplitude.
The QT interval normally decreases with increasing heart rates and lengthens with slower heart rates. A failure to shorten the QT interval during increased heart rates is a response consistent with long QT syndrome. The QT interval can vary up to 100 msec over the course of the day, felt largely due to autonomic tone. It is longer in the night compared with the morning and daytime hours.
There are many methods to measure the corrected QT interval. Three commonly used methods are as follows:
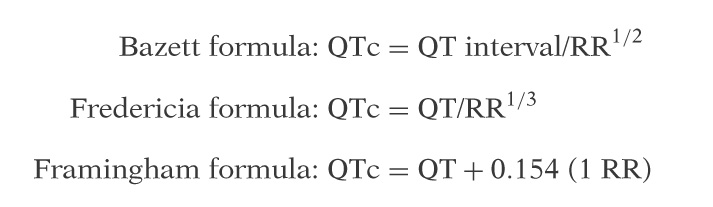
The most widely used formula to determine the QT interval corrected for heart rate is the Bazett formula. This formula is limited by overcorrection at high heart rates and undercorrection at low rates.
Special Circumstances
Atrial Fibrillation
There is no standard method for assessing the QT interval during atrial fibrillation (AF). Options include averaging ten consecutive QT intervals or the longest and shortest QT interval on an ECG.
Bundle Branch Block
The prolongation in the QRS interval may lead to prolonged QT intervals which are not solely due to abnormal repolarization. A typical correction normalizes the QRS to 100 or 110 msec—therefore, if the QRS is 160 msec, 50 msec is subtracted from the QT interval.
Ambulatory Arrhythmia Monitoring
Ambulatory arrhythmia monitoring is used most often for the identification of symptomatic arrhythmias to determine the cause of palpitations, the documentation of asymptomatic arrhythmias including the determination of the cause of syncope, the identification of nonsustained ventricular tachycardia (NSVT) for sudden death risk assessment, or the cause of stroke such as AF (see Table 17-1). These devices are also useful for the assessment of heart rate during chronic arrhythmias such as AF.
Holter monitors are large devices which are generally worn for 48 hours. They record continuously and save all data for the entirety of the monitoring period. Patients can keep a diary of their symptoms to correlate with the arrhythmias identified with scanning of the 48-hour monitoring period. These
devices are ideal for monitoring the heart rate in chronic AF or documenting chronotropic competence. They are less helpful for the diagnosis of palpitations or syncope given the short duration of monitoring.
devices are ideal for monitoring the heart rate in chronic AF or documenting chronotropic competence. They are less helpful for the diagnosis of palpitations or syncope given the short duration of monitoring.
TABLE 17-1 Ambulatory Monitoring Arrhythmia Devices and Common Indications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree