The objective of this study was to evaluate inert gas rebreathing (IGR) reliability in cardiac output (CO) measurement compared with Fick method and thermodilution. IGR is a noninvasive method for CO measurement; CO by IGR is calculated as pulmonary blood flow plus intrapulmonary shunt. IGR may be ideal for follow-up of patients with pulmonary hypertension (PH), sparing the need of repeated invasive right-sided cardiac catheterization. Right-sided cardiac catheterization with CO measurement by thermodilution, Fick method, and IGR was performed in 125 patients with possible PH by echocardiography. Patients were grouped according to right-sided cardiac catheterization–measured mean pulmonary and wedge pressures: normal pulmonary arterial pressure (n = 20, mean pulmonary arterial pressure = 18 ± 3 mm Hg, pulmonary capillary wedge pressure = 11 ± 5 mm Hg), PH and normal pulmonary capillary wedge pressure (PH-NW, n = 37 mean pulmonary arterial pressure = 42 ± 13 mm Hg, pulmonary capillary wedge pressure = 11 ± 6 mm Hg), and PH and high pulmonary capillary wedge pressure (PH-HW, n = 68, mean pulmonary arterial pressure = 37 ± 9 mm Hg, pulmonary capillary wedge pressure = 24 ± 6 mm Hg). Thermodilution and Fick measurements were comparable. Fick and IGR agreement was observed in normal pulmonary arterial pressure (CO = 4.10 ± 1.14 and 4.08 ± 0.97 L/min, respectively), whereas IGR overestimated Fick in patients with PH-NW and those with PH-HW because of intrapulmonary shunting overestimation in hypoxemic patients. When patients with arterial oxygen saturation (SO 2 ) ≤90% were excluded, IGR and Fick agreement improved in PH-NW (CO = 4.90 ± 1.70 and 4.76 ± 1.35 L/min, respectively) and PH-HW (CO = 4.05 ± 1.04 and 4.10 ± 1.17 L/min, respectively). In hypoxemic patients, we estimated pulmonary shunt as Fick − pulmonary blood flow and calculated shunt as: −0.2423 × arterial SO 2 + 21.373 L/min. In conclusion, IGR is reliable for CO measurement in patients with PH with arterial SO 2 >90%. For patients with arterial SO 2 ≤90%, a new formula for shunt calculation is proposed.
A noninvasive method for cardiac output (CO) measurement by inert gas rebreathing (IGR) has been proposed and validated in healthy subjects and patients with heart failure. IGR calculates CO as the sum of pulmonary blood flow and intrapulmonary shunt; IGR relies on proper alveolar gas mixing for pulmonary blood flow measurement and estimation of intrapulmonary shunt based on the assumption of a constant oxygen saturation (SO 2 ) value in the pulmonary capillaries. Both measurements may be challenging in patients with pulmonary hypertension (PH) who have an abnormal ventilatory perfusion match and a significant intrapulmonary shunt. Therefore, there is a clear need to validate the IGR technique in patients with PH. To that end, we simultaneously measured CO by IGR, thermodilution, and direct Fick method during right-sided cardiac catheterization in a sizable group of patients with PH.
Methods
The present study involved 125 patients consecutively referred to our Pulmonary Hypertension Unit with an echocardiographic evaluation suggestive of PH. To confirm the diagnosis of PH, all subjects underwent right-sided cardiac catheterization, which included simultaneous CO determination by 3 techniques: thermodilution, direct Fick method, and IGR. Patients with severe chronic pulmonary disease at spirometry (forced expiratory volume <60% of predicted and vital capacity <60%), congenital heart disease, or those with intracardiac shunt (echocardiography) were excluded because of possible bias of CO measurement with IGR. The patients were divided into 3 groups according to their pulmonary hemodynamic pattern: (1) patients with PH and normal capillary wedge pressure (PH-NW; mean pulmonary arterial pressure ≥25 mm Hg and pulmonary capillary wedge pressure <15 mm Hg), such as those belonging to classes 1 and 4 of the European Society of Cardiology guideline classification of PH 3; (2) patients with high values of both pressures (PH-HW; mean pulmonary arterial pressure ≥25 mm Hg and pulmonary capillary wedge pressure ≥15 mm Hg; class 2); and (3) patients in whom PH was not confirmed at right-sided cardiac catheterization. Patients with confirmed PH at right-sided cardiac catheterization underwent spirometry, pulmonary tomography, laboratory tests, and abdominal ultrasonography.
The study was approved by our institution’s scientific and ethical committees, and all patients gave written informed consent.
Right-sided cardiac catheterization was performed through a right femoral vein. A 7Fr, balloon-tipped, flow-directed Swan Ganz catheter was positioned with fluoroscopic guidance in the pulmonary artery.
Regardless of the technique, all CO measurements were performed while patients were in the supine position; the invasive and noninvasive measurements were done in a random order one after the other by 2 different physicians. Baseline hemodynamic was recorded after an adequate patients’ rest time; the zero reference level (midchest) was checked at the beginning of pulmonary pressure measurement, and the wedge pressure was obtained by the mean value of occlusion artery trace. All measurements were performed without supplemental oxygen. CO measurements required no more than 20 minutes.
Thermodilution CO measurement was performed by injecting 10 ml of cold saline solution into the right atrium (Prucka CardioLab; GE, Milwaukee, Wisconsin). The reported data are an average of 3 measurements agreeing within 10%.
CO was measured with the direct Fick method using the following formula: CO = VO 2 /(CaO 2 − CvO 2 ), where VO 2 is the rest averaged VO 2 of 3-minute measurements directly assessed by IGR; CaO 2 and CvO 2 are the O 2 content in blood samples directly collected from a systemic artery and the pulmonary artery, respectively.
IGR technique (Innocor; Innovision, Odense, Denmark) has been previously reported in detail. CO was calculated by the sum of pulmonary blood flow and shunt flow, the latter estimated using the following formula: shunt flow = 1/[(CaO 2 − CcO 2 )/VO 2 + 1/pulmonary blood flow] − pulmonary blood flow. CaO 2 and CcO 2 are the O 2 content in peripheral artery and capillary lung blood, respectively, and they are equal to the product of a constant (0.000139), hemoglobin, measured in a venous blood sample, and arterial and capillary SO 2 ; the latter was assessed by peripheral arterial blood sample for CaO 2 , and pulmonary capillary SO 2 was assumed to be equal to 98%. The final values of CO and pulmonary blood flow used were an average of 2 or 3 measurements agreeing within 10%.
Data are shown as mean ± SD, unless otherwise specified. CO and shunt values obtained by the Fick method, thermodilution, and IGR were compared in pairwise manner using the Student t test. Analyses were performed using the standard statistical software (SPSS, version 18.0; IBM, Chicago, Illinois). Agreement between the Fick method and IGR was assessed with the graphical method described by Bland and Altman including confidence intervals.
Results
From January 2008 to November 2012, 125 consecutive patients with an echocardiographic evaluation suggestive of PH were enrolled in the study. Thirty-seven patients had PH-NW, 68 had PH-HW, and 20 had normal pulmonary arterial pressure ( Table 1 ). All patients underwent right-sided cardiac catheterization without complications. The hemodynamic features are detailed in Tables 2 and 3 . In patients with PH, either with elevated or normal pulmonary wedge pressure, IGR overestimated CO ( Table 3 ). Conversely, in patients with normal pulmonary arterial pressure, the agreement among CO measurements by IGR, Fick, and thermodilution was elevated. Figure 1 reports the Bland and Altman correlation of IGR versus Fick CO measurements in the 3 groups. Similar results were obtained by comparing IGR versus thermodilution CO determination. We estimated intrapulmonary shunt as Fick CO − pulmonary blood flow and IGR CO − pulmonary blood flow ( Table 3 ). However, because shunt estimation by IGR assumed a pulmonary capillary SO 2 equal to 98%, a value which is likely overestimated in patients with severe hypoxemia, we separately analyzed patients with arterial SO 2 >90% and ≤90%.
| Variable | Normal PAP (n = 20, 16%) | PH-HW (n = 68, 54%) | PH-NW (n = 37, 30%) |
|---|---|---|---|
| Men/Women | 8/12 | 30/38 | 13/24 |
| Weight (kg) | 69 ± 11 | 71 ± 20 | 71 ± 15 |
| Height (cm) | 167 ± 10 | 164 ± 18 | 165 ± 7 |
| Age (yr) | 66 ± 14 | 66 ± 12 | 54 ± 16 |
| PAPs (mm Hg) | 43 ± 11 | 54 ± 16 | 67 ± 18 |
| LVEF (%) | 53 ± 14 | 53 ± 15 | 65 ± 9 |
| Variable | Normal PAP (n = 20, 16%) | PH-HW (n = 68, 54%) | PH-NW (n = 37, 30%) |
|---|---|---|---|
| Mean pulmonary arterial pressure (mm Hg) | 18 ± 3 | 37 ± 9 | 42 ± 13 |
| Systolic pulmonary arterial pressure (mm Hg) | 28 ± 5 | 57 ± 16 | 69 ± 22 |
| Diastolic pulmonary arterial pressure (mm Hg) | 12 ± 4 | 24 ± 7 | 28 ± 9 |
| Wedge pressure (mm Hg) | 11 ± 5 | 24 ± 6 | 11 ± 6 |
| Pulmonary vascular resistance (WU) | 2 ± 1 | 3 ± 2 | 7 ± 4 |
| Variable | Normal PAP (n = 20, 16%) | PH-HW (n = 68, 54%) | PH-HW SO 2 >90% (n = 61, 49%) | PH-NW (n = 37, 30%) | PH-NW SO 2 >90% (n = 32, 26%) |
|---|---|---|---|---|---|
| Fick (L/min) | 4.10 ± 1.14 | 4.09 ± 1.13 | 4.10 ± 1.17 | 4.80 ± 1.50 | 4.76 ± 1.35 |
| Therm (L/min) | 4.16 ± 1.15 | 4.05 ± 1.11 | 4.02 ± 1.12 | 4.86 ± 1.83 | 4.86 ± 1.84 |
| IGR (L/min) | 4.08 ± 0.97 | 4.47 ± 2.32 | 4.05 ± 1.04 | 5.43 ± 2.60 | 4.90 ± 1.70 |
| PBF (L/min) | 3.56 ± 0.91 | 3.48 ± 0.85 | 3.47 ± 0.87 | 4.05 ± 1.33 | 4.01 ± 1.34 |
| Shunt [Fick − PBF] (L/min) | 0.54 ± 0.62 | 0.60 ± 0.76 | 0.64 ± 0.77 | 0.76 ± 0.89 | 0.75 ± 0.78 |
| Shunt [IGR − PBF] (L/min) | 0.52 ± 0.37 | 0.98 ± 2.07 | 0.58 ± 0.53 | 1.38 ± 1.90 | 0.89 ± 0.85 |
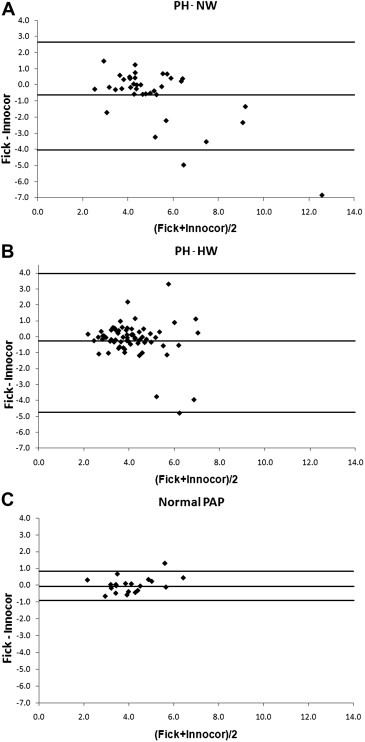
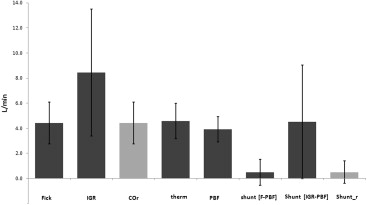
We identified 12 patients with arterial SO 2 ≤90%, 5 with PH-NW and 7 with PH-HW. Figure 2 graphically shows the difference in CO measurements among IGR, Fick, and thermodilution in these 12 patients separately. These data support the concept that the difference found in CO measurement between Fick method and IGR is due to shunt overestimation by IGR. Indeed, excluding patients with arterial SO 2 ≤90%, the correspondence of CO measurements by IGR, Fick, and thermodilution significantly improved ( Table 3 and Figure 3 ). Reproducibility of CO measurement by IGR was 15% in the total population and 10% in patients with arterial SO 2 >90%. Moreover, in patients with arterial SO 2 >90%, the agreement between intrapulmonary shunts calculated as Fick CO − pulmonary blood flow and IGR CO − pulmonary blood flow improved ( Table 3 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


