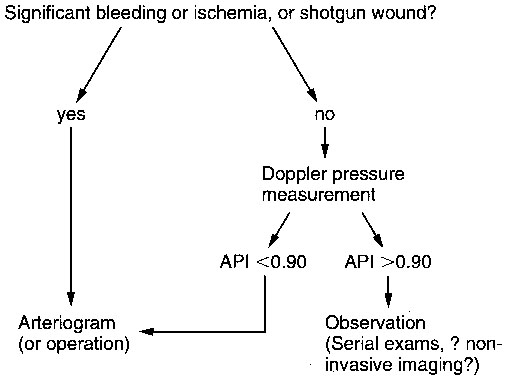
Some groups used an ankle pressure index (ratio of highest ankle arterial pressure to arm arterial pressure; ABI) of 0.90 as a threshold value below which the presence of an arterial disruption was possible and above which such an injury was unlikely (Figure 1). Others promoted the even greater sensitivity of an ABI of 1.0, accepting that such an approach resulted in the performance of many more negative arteriograms. Most importantly, whichever ABI threshold was chosen, these studies validated the use of a simple bedside diagnostic test, using a blood pressure cuff and a hand-held Doppler, to assess patients with potential occult penetrating arterial trauma of the extremities.
Nonarteriographic Diagnosis of Penetrating Vascular Trauma
Arterial Pressure Measurements
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine