16 Non-Neuroendocrine Carcinomas (Excluding “Sarcomatoid” Carcinoma) and Salivary Gland Analog Carcinomas in the Lung
Carcinoma of the lung is a growing public health problem of worrisome proportions, not only in the United States but also internationally.1–5 The American Cancer Society has estimated that more than 170,000 new cases of lung cancer will occur each year in the United States in the foreseeable future. This unfortunate reality reflects the continuing use of cigarettes, cigars, and pipes by a significant fraction of the world population and the undeniable causal relationship between inhaled tobacco smoke and pulmonary carcinoma.1–7 To make matters worse, it has been shown that persons who are in constant and close proximity to heavy smokers, either at home or in the workplace, inhale sufficient “sidestream” smoke to place them at definite risk for lung cancer even if they have never smoked themselves.6,8,9 The potential pathogenetic influence of other proposed etiologic agents (e.g., human papillomavirus, radon, pneumoconiosis-related minerals, hereditary syndromes) on pulmonary carcinogenesis also continues to undergo analysis.3,10–21 Women now have an incidence of lung cancer on a rough numerical parity with men, and the mortality rate in both sexes is so high that lung cancer represents the leading worldwide cause of death related to malignancy.2,5,6
Nosology of Lung Cancer and Diagnostic Effects of Sampling Methods
Seventy-five years ago, the first attempt at morphologic classification of lung cancer was undertaken by Marchesani.10 This scheme, outlining the now-classic categories of squamous cell carcinoma (SCC), adenocarcinoma (ACA), and small cell “undifferentiated” and large cell “undifferentiated” carcinomas, is still widely recognized and has gone through several iterations over the ensuing decades. Recently, a pragmatic, clinically attuned movement has been enjoined wherein a more simplified system was embraced, dividing malignant epithelial tumors of the lung into “small cell” and “non–small cell” carcinomas. At the same time, research by pathologists has resulted in ever-greater refinement of morphologic categorization, and the interface between the practical needs of the operating suite and data generated in the clinical laboratory has become problematic. In light of this situation, a prognostically oriented nosologic scheme for lung cancer was devised by the Veterans Administration Lung Group in 1991.22 It has since been modified by other organizations, most notably, the World Health Organization.23
Whether a pathologist elects to use one or another of these systems is a decision that should be made after consultation with clinical colleagues. In any event, nonstandard designations for pulmonary carcinomas (i.e., those that are not sanctioned by the World Health Organization)23 should be well defined in surgical pathology reports, with pertinent references provided in cases that are particularly uncommon or conceptually contentious.
A particular problem that must be recognized by everyone involved in treating lung cancer is the common heterogeneity that it may demonstrate at a light microscopic level. The literature is now well supplied with reports of admixtures of virtually all of the lung carcinoma histotypes in the same tumor mass.3,12,24–26 An analysis by Roggli and colleagues27 demonstrated such heterogeneity in fully 66% of a consecutive series of lung cancers, and others have reported similar findings. This biologic diversity may attain prognostic importance in the future, particularly in light of recent work that appears to affirm the effect of histologic features on tumor evolution.28 Neoplastic heterogeneity is a practical diagnostic problem for surgeons and medical oncologists, because small biopsies often do not represent “divergent” tumor elements as a consequence of sampling bias. At a time when ever more limited methods of tissue procurement are being advanced, it is clear that substantial discrepancies will be observed between biopsy results and findings of resection specimens in the surgical pathology laboratory.29,30 That is not to imply that such techniques as fine-needle aspiration biopsy should not be used, because they are extremely helpful in planning therapy in many cases. Nonetheless, the potential limitations of all sampling procedures must be weighed carefully against their benefits.
Clinicopathologic Features of Non-Neuroendocrine Pulmonary Carcinomas, Excluding “Sarcomatoid” Carcinoma
Squamous Cell Carcinoma
Probably because of changes in the smoking habits of the public, with a greater preference for filtered cigarettes in the last 35 years,7 SCC is no longer the most common type of lung cancer and has been eclipsed by ACA in recent years.25,31 However, SCC has retained its classic clinicopathologic attributes. These include a tendency for multifocal but clonal in situ disease in the bronchial mucosa, often preceding the appearance of a discrete mass by several years, and a propensity to arise in large central airways proximal to the subsegmental bronchi. Because of the common presence of an endobronchial tumor mass, obstructive pneumonia is a relatively common accompaniment of this neoplasm, but it is not pathognomonic. “Pure” SCC may originate in the peripheral pulmonary parenchyma as well, and rare examples are even subpleural.3
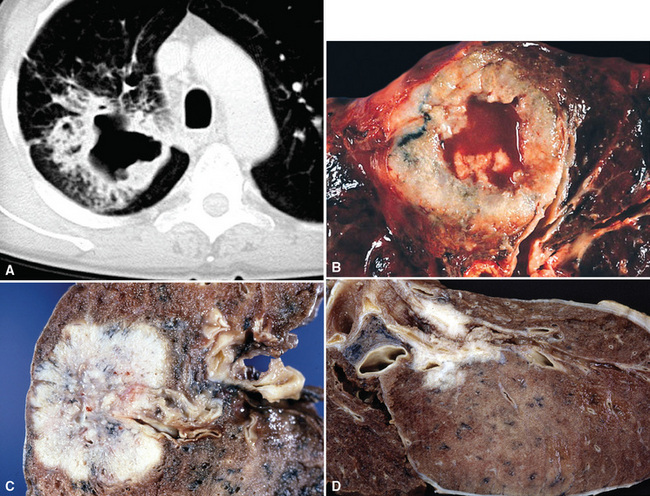
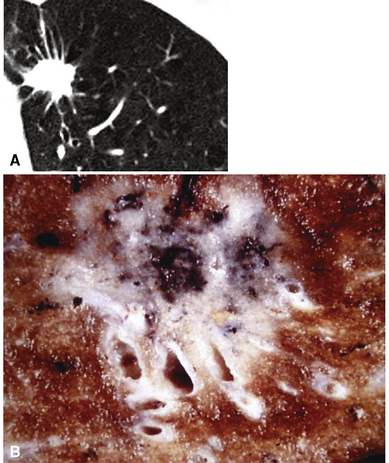
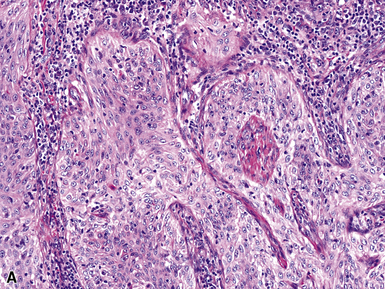
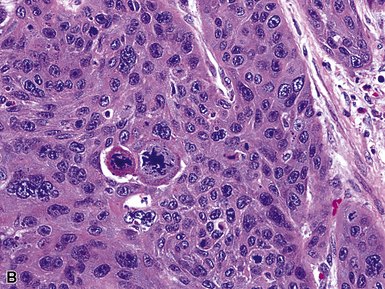
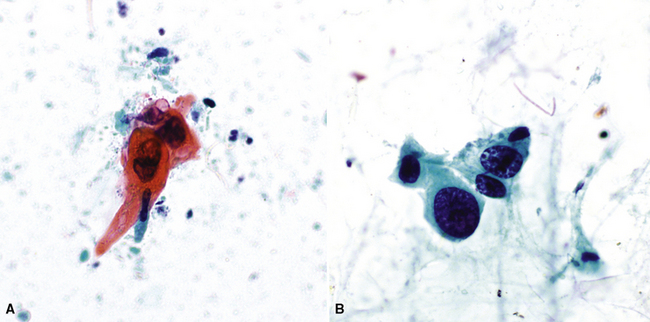
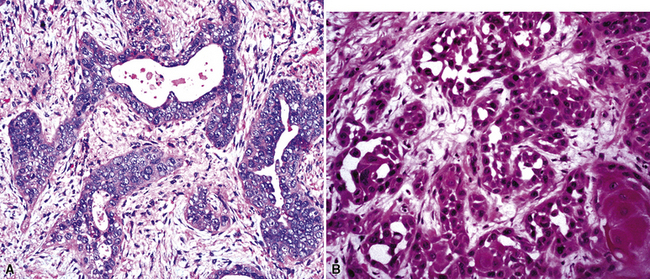
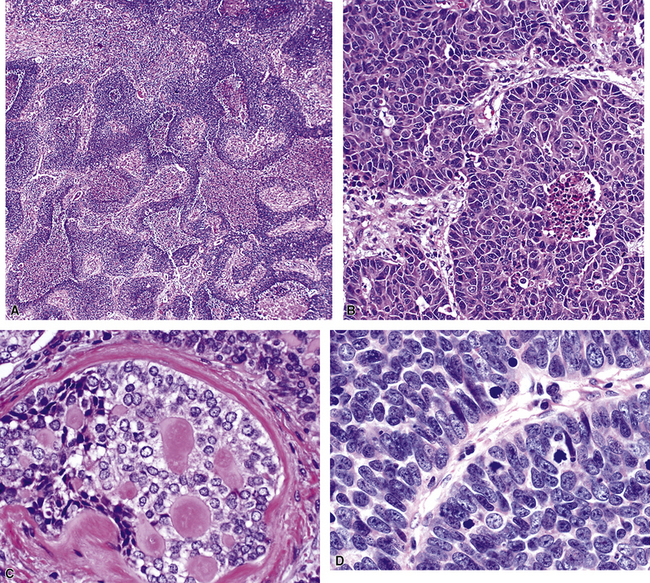
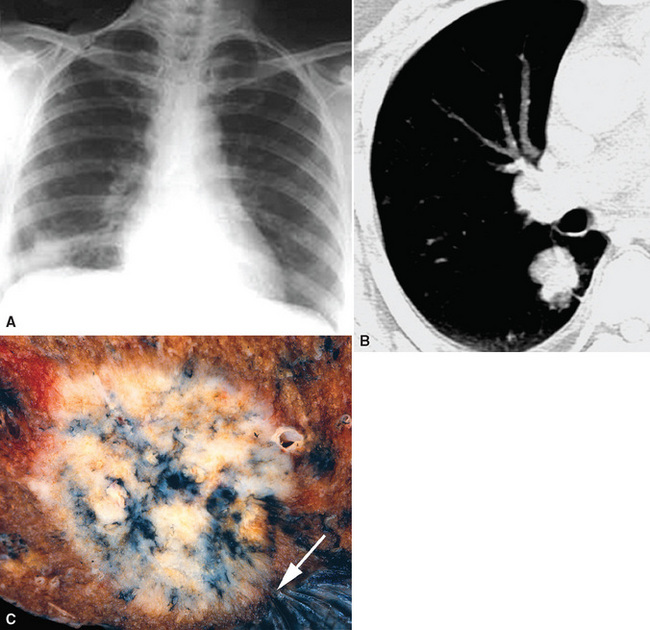
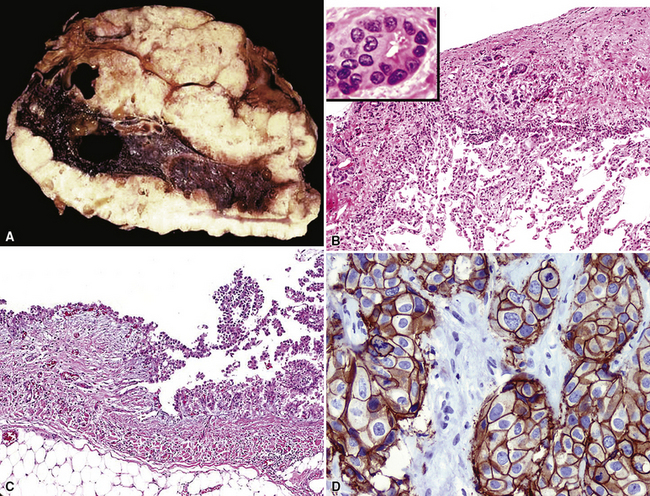
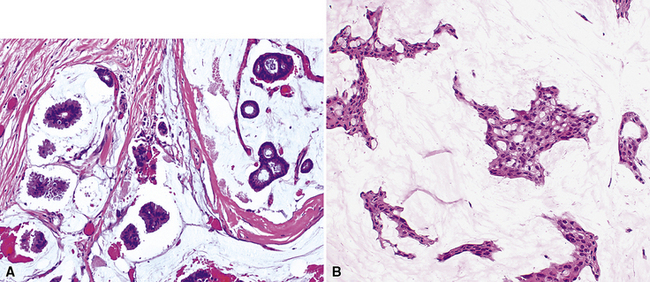
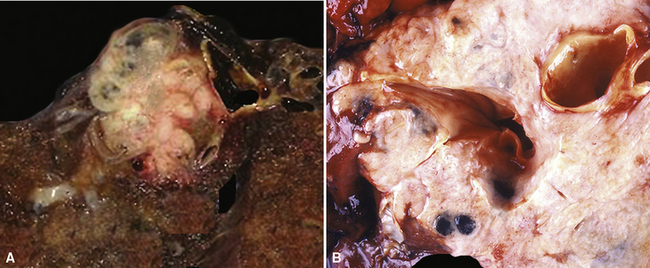
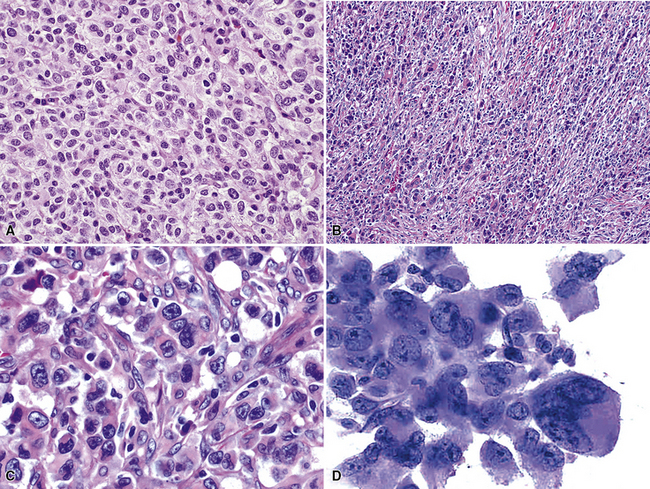
Squamous cell cancer of the lung has an irregular, often friable, gray-white cut surface, commonly showing a large area of central necrosis, with or without cavitation (Fig. 16-1). The surrounding pulmonary parenchyma is frequently tethered to the mass, giving it a “spiculated” appearance that may be well seen on radiographic images (Fig. 16-2). Microscopically, SCC is defined by its resemblance to stratified squamous epithelium of the upper airway, but with disordered architectural and cytologic maturation (Figs. 16-3 to 16-6). Anucleate keratin and squamous pearls are observed in better differentiated lesions, which account for a minority of pulmonary carcinomas. Poorly differentiated SCC may be extremely difficult for the pathologist to distinguish from high-grade ACAs, small cell carcinomas, or large cell undifferentiated carcinomas (LCCs), because they commonly take the form of rather nondescript proliferations of primitive epithelioid cells of varying size, arranged in nests and sheets, with no other distinguishing features. In the absence of special studies, one may have to use the default terminology of “poorly differentiated carcinoma, not further specified,” in the frozen section laboratory and in small biopsies of such lesions. Recognized and distinct subtypes of poorly differentiated SCC include spindle cell and pleomorphic (sarcomatoid) forms32–35 (see Chapter 14); adenoid-acantholytic (pseudoglandular) variants (Fig. 16-7)36; a pseudovascular (angiosarcoma-like) subtype (Fig. 16-8)36,37; “lymphoepithelioma-like” carcinoma (Fig. 16-9)38; and a basaloid form (Fig. 16-10) (“small cell squamous carcinoma” or “basaloid squamous cell carcinoma”)39 that is analogous to primary poorly differentiated SCC of the anorectum, hypopharynx, thymus, and other anatomic sites. Other than presenting special problems in microscopic differential diagnosis, these tumor variants have no singular clinical significance in comparison with other high-grade carcinomas.
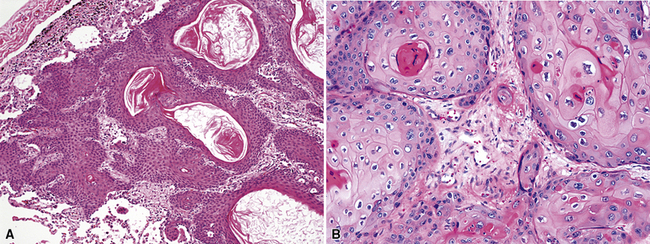
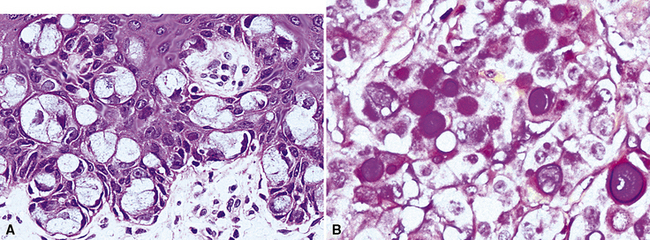
Figure 16-3 A and B, Photomicrographs of well-differentiated squamous carcinoma showing obvious keratinization.
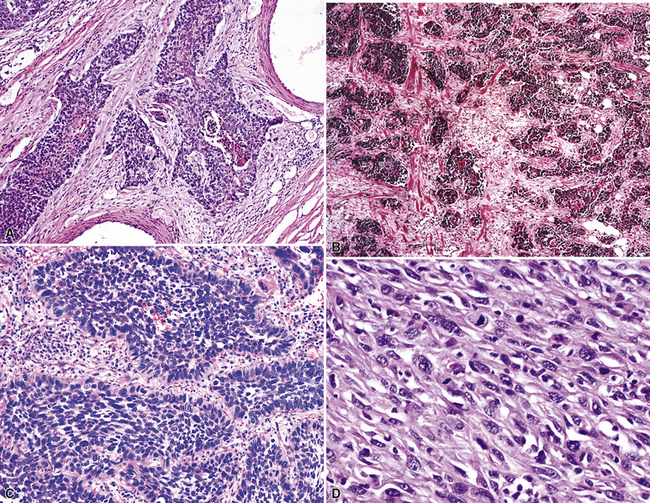
Figure 16-5 A, Poorly differentiated squamous cell carcinoma (PDSCC) showing only focal keratinization and predominant composition by primitive epithelial cells. B, PDSCC comprising groups of relatively primitive polygonal cells invading the soft tissue of the chest wall. C, Only very focal keratinization is apparent in this PDSCC. D, PDSCC with sarcomatoid features, presenting difficulty in recognition of the lesion as epithelial (see Chapter 14).
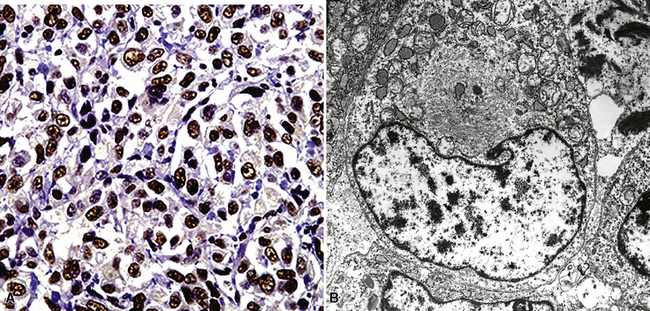
For unknown reasons, SCC has a greater association with selected hereditary syndromes than do other forms of lung carcinoma.11–21 These conditions are extremely rare causes of pulmonary neoplasia, but they include such disorders as Muir-Torre syndrome, von Hippel-Lindau disease, and dysplastic nevus (“atypical mole”) syndrome. In one of them—Muir-Torre syndrome—immunohistochemical analyses can be done for the absence of nucleic acid mismatch repair proteins in the tumor cells. The three most commonly assessed gene products are MLH1, MSH2, and MSH6 (Figs. 16-11 and 16-12).
Nonbronchioloalveolar Adenocarcinomas
As stated earlier, ACA has now successfully eclipsed SCC as the most common form of monodifferentiated lung cancer. In North America and Europe, most ACAs are predominantly peripheral parenchymal masses; however, interestingly, histologically identical lesions in India and Asia are as likely to be central as peripheral in location. Grossly, ACA typically has an irregularly lobulated configuration, with a gray-white cut surface (Fig. 16-13). Anthracotic pigment is commonly entrapped in the tumor mass as well, but foci of necrosis and hemorrhage are seen only in large (>5 cm) lesions. A relationship to tubular airways is only rarely obvious. Close inspection may also demonstrate the presence of “satellite” nodules around the main tumor mass; however, this phenomenon may be a reflection of the tendency for pulmonary ACA to be synchronously or metachronously multifocal, either in one lobe of the lung or in both lungs. The latter statement applies particularly to a special subtype of ACA, bronchioloalveolar carcinoma (BAC; discussed later). One peculiar and uncommon gross presentation of pulmonary ACA that merits special mention is its “pseudomesotheliomatous” form, wherein the pleurotropic growth of extremely peripheral intrapulmonary tumors creates a “rind” of tumor tissue surrounding the lung (Fig. 16-14). This virtually perfectly simulates the appearance of mesothelioma, both intraoperatively and radiographically.40–42
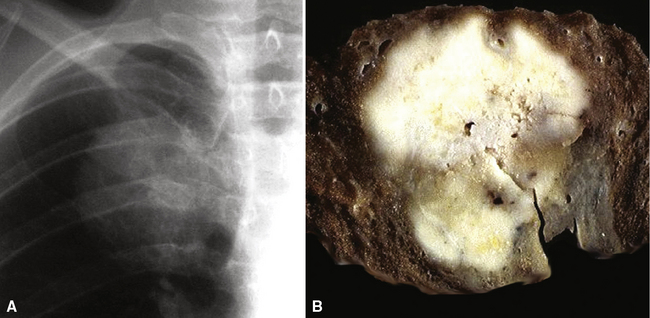
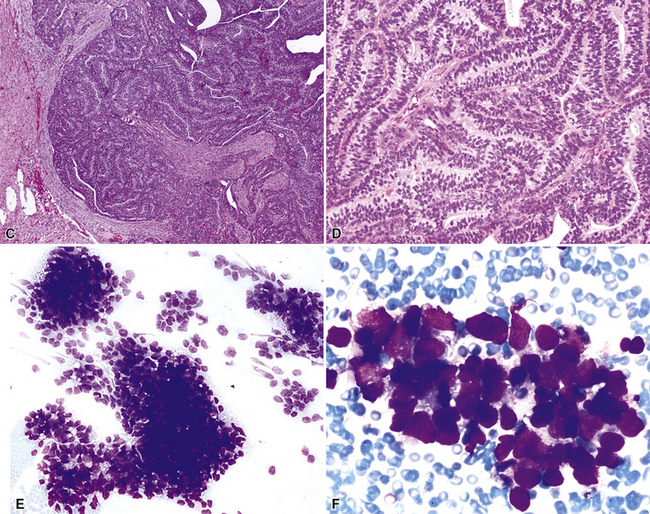
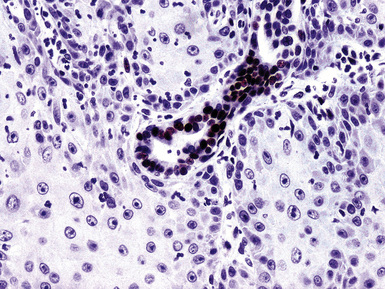
Figure 16-18 A, “Fetal” adenocarcinoma of the lung is considered to be in the same general family of tumors as pulmonary “blastoma,” and is shown here in an adult patient as a peripheral nodule in the right upper lung field on a plain-film radiograph. B, The resected tumor is a solid, relatively well-demarcated, and homogeneous mass. C and D, Microscopically, fetal adenocarcinoma comprises closely apposed glandular arrays made up of compact columnar cells, resembling those seen in embryonic lungs. E and F, Fine-needle aspiration specimens of fetal adenocarcinoma show small cells with high nucleocytoplasmic ratios, dispersed chromatin, and a tendency to surround small central spaces. Cytologic differential diagnosis includes neuroendocrine and neuroectodermal lesions (see Chapter 13).
(A and B, Courtesy of Dr. Samuel A. Yousem, Pittsburgh, PA. E and F, Courtesy of Dr. Kim Geisinger, Winston-Salem, NC).
However, more variants exist, such as clear cell and enteric (intestinal-like; Fig. 16-22).47–52 In some cases, because of the overlap between these histologic groups and the appearance of metastatic ACAs in the lung, it may be extremely difficult for the pathologist to separate primary from secondary lesions. This is particularly true of enteric and signet ring cell tumors, which can closely imitate the attributes of gastric or colorectal carcinomas (see Chapter 17). Psammoma bodies can also be seen in primary papillary ACAs of the lung,43,53 and these structures therefore raise the question of whether one is instead viewing a solitary metastasis from an occult tumor of the thyroid, ovary, or another location wherein psammomatous carcinomas are potentially found. Needless to say, in cases featuring multifocality of ACA in more than one lobe, this problem is even more striking. Special studies, including electron microscopy and immunohistology, are helpful in resolving this differential diagnosis. Ultimately, however, diagnostic reliance is also placed on such banal characteristics as peritumoral fibrosis and inflammation, which are more common in primary pulmonary lesions than in metastases.
Pulmonary ACA may rarely involve the bronchial epithelium diffusely in a pagetoid fashion (Fig. 16-23).54 Whether this represents intraepithelial spread of the tumor or multifocal synchronous growth is an open question, but pagetoid lesions are excruciating management problems because of the difficulty in obtaining tumor-free bronchial margins.
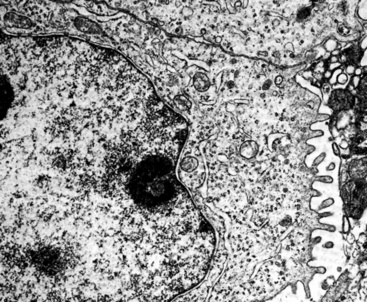
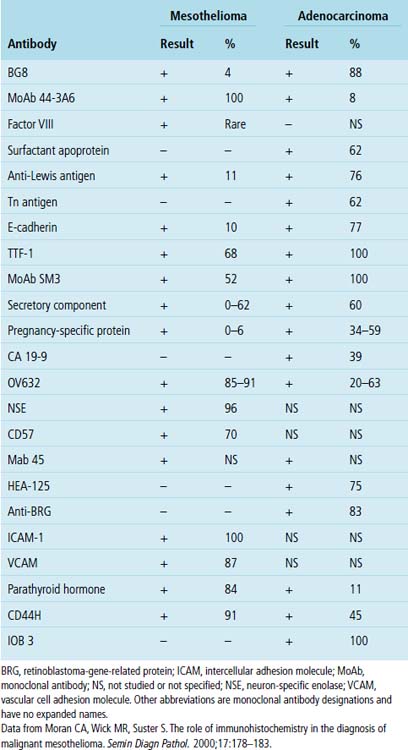
“Pseudomesotheliomatous” (pleurotropic) ACAs are indeed separable from true mesotheliomas using adjuvant pathologic techniques, particularly immunophenotyping and electron microscopy (Figs. 16-24 and 16-25 and Table 16-1).55 Nonetheless, whether this exercise has any more than academic significance is an open question. Available therapies for both of these tumor types are suboptimal, and the only real significance of the differential diagnosis may be a medicolegal one. In the absence of asbestosis, pleurotropic ACA has no proven causal relationship to asbestos exposure.
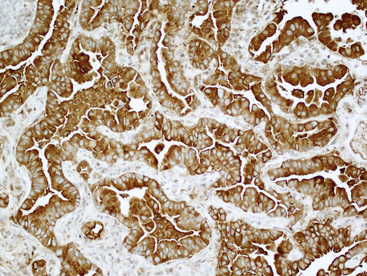
Figure 16-24 The tumor depicted in Figure 16-14 shows diffuse immunoreactivity for carcinoembryonic antigen, as expected in most adenocarcinomas of the lung but not in mesotheliomas.
Bronchioloalveolar Carcinoma
Bronchioloalveolar carcinoma of the lung was initially described in the 1800s, but was most fully characterized as a distinct entity by Liebow in 1960.56 Since that time, BAC has been the subject of intense interest and controversy. In particular, the pathologic criteria that apply to its diagnosis and how its histologic attributes relate to prognosis represent perhaps the two most contentious issues.57–65
There are no particular distinguishing demographic features associated with BAC vis-à-vis other ACAs of the lung. They tend to occur in elderly individuals, with an essentially equal distribution by sex.58,65 Contrary to reports in the 1970s63—before such phenomena as “passive” tobacco exposure were recognized—there is a definite relationship between cigarette smoking and the genesis of this tumor, as is true of virtually all pulmonary carcinomas. Nonetheless, BAC is indeed over-represented (with regard to other histotypes of lung cancer) in patients who have never smoked and who have never lived with smokers. This point has raised the issue of whether other etiologic factors—in particular, infection with human papillomavirus—might account for the genesis of some BACs.
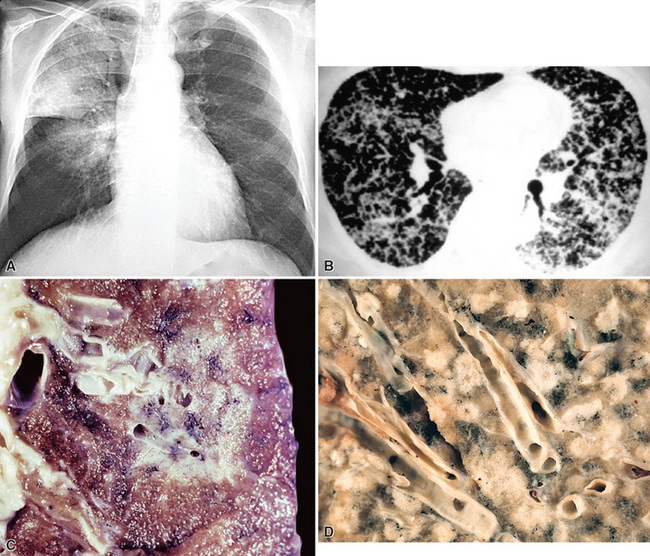
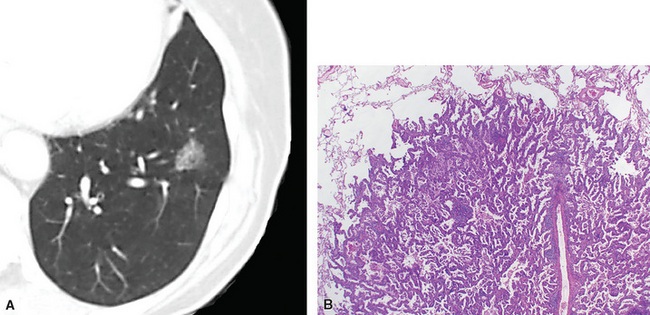
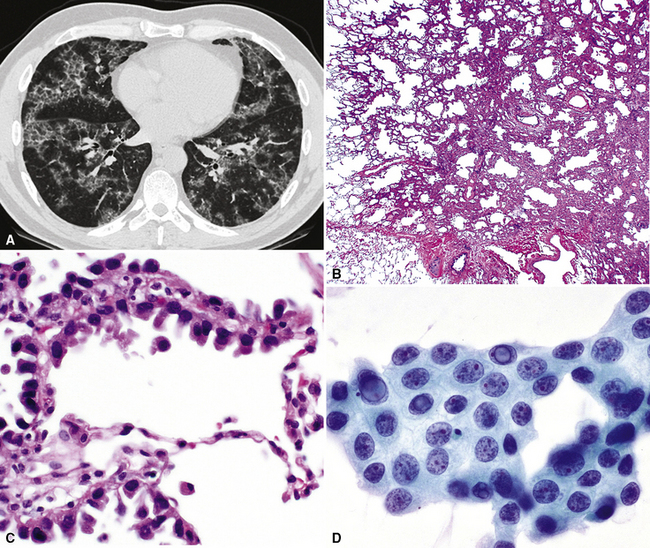
Radiologically and clinically, three discrete subsets of patients with BAC are recognized.65,66 These include individuals who have chest radiographic findings and clinical symptoms suggesting pneumonia (fever, productive cough, and lobar or segmental consolidation; Fig. 16-26) as well as some patients with a solitary peripheral mass lesion (Fig. 16-27) and others with multiple rounded densities throughout one or both lung fields (Fig. 16-28). On computed tomograms, the latter lesions may assume a “Cheerio” shape, in that they commonly demonstrate small central areas of cavitation. Hence, BAC may simulate an infectious disease, represent a nondescript “coin” lesion of the lung, or imitate the pattern of metastases to the lung from an occult visceral neoplasm.
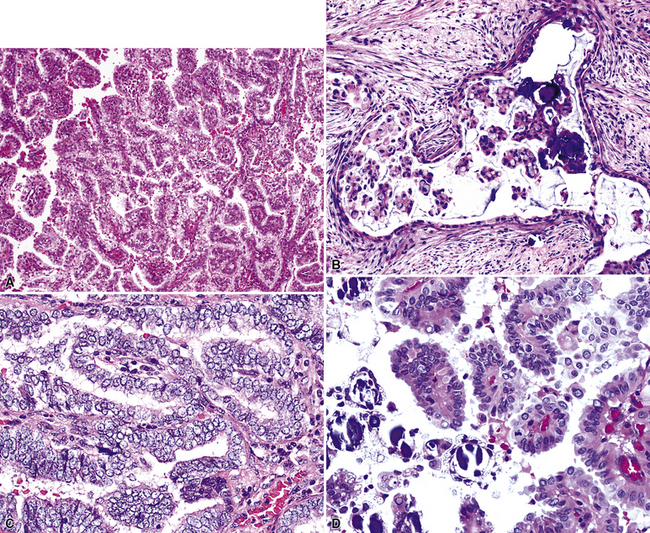
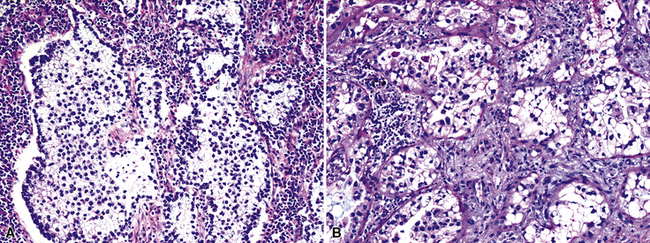
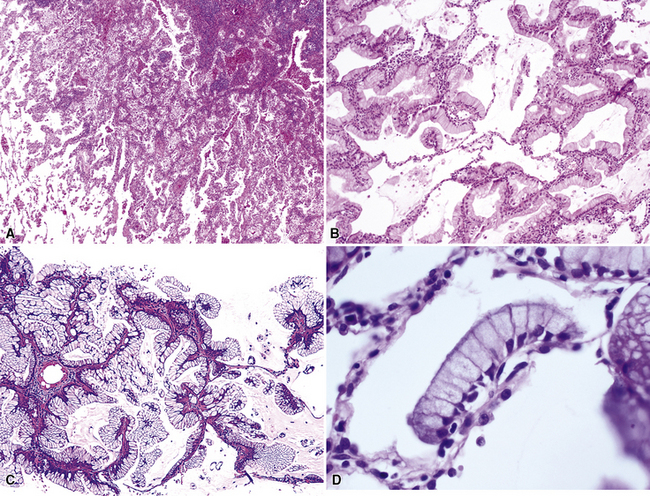
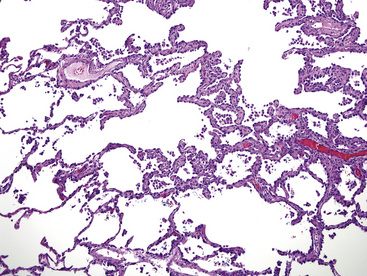
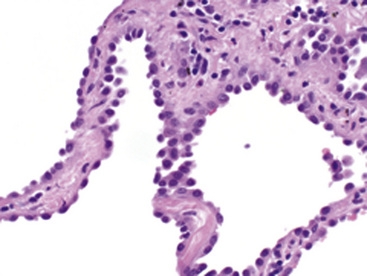
Histologically, two distinct cytologic subtypes of BAC are recognized: mucinous and nonmucinous.57,58,62 These are of importance because of their clinical associations. Mucinous tumors (Fig. 16-29) are those that tend to assume a pseudopneumonic or multifocal/multinodular clinical appearance, whereas nonmucinous BAC (Fig. 16-30) is more commonly a solitary lesion. Furthermore, stage for stage, nonmucinous variants may show a more favorable clinical evolution.62,67 The criteria for the distinction of BAC from “ordinary” pulmonary ACAs continue to be debated. In accord with current convention, we restrict the use of this diagnosis to neoplasms that demonstrate a mantling of pre-existing air spaces (“lepidic” or noninvasive growth) by single layers or limited strata and micropapillae of only modestly atypical cuboidal or columnar epithelial cells, with or without intracellular or extracellular mucin production. Intranuclear inclusions of cytoplasm containing surfactant proteins are also common.68 Save for mucin production, such characteristics are shared by both forms of BAC, mucinous and nonmucinous (serous). Septal widening and sclerosis may be seen, especially with nonmucinous BAC, but there must be no desmoplasia or inflammation within or around the lesion if it is to be considered a bona fide BAC. Caution should be exercised in diagnosing BACs with central sclerosis because this is often a site of subtle early invasion. This demanding definition differs from that of some other observers, who have accepted the existence of a “sclerosing” BAC subtype.69 Justification for more narrow requirements is gained from biologic data, which show worse behavior of “sclerosing” or “invasive” BAC than of nonfibrotic tumors.57,70,71 Indeed, Clayton,58 who devoted much attention to BAC, clearly stated that bronchioloalveolar carcinomas with sclerosis should be classified with other peripheral ACAs.
Another traditional point of discussion pertaining to the microscopic features of BAC (particularly its mucinous form) is that this neoplasm is said to disseminate within the lung by “aerogenous” means. That is to say, tumor cells are believed to detach from a “mother lesion” and spread to other foci in the pulmonary parenchyma by the process of inhalation and exhalation. Some molecular analyses, however, have cast doubt on that premise and instead suggest that the lesions are multiclonal.72
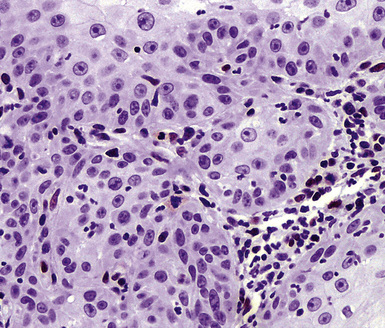
Other lesions that may be confused pathologically with BAC include foci of florid type II pneumocytic hyperplasia surrounding areas of diffuse alveolar damage73 and interstitial fibrosing pneumonitides or organizing pulmonary infarcts74; the proliferation known as “atypical adenomatous alveolar hyperplasia” (discussed later)75; and the unicentric neoplasms known as “papillary alveolar adenoma” and “sclerosing hemangioma.”76 The latter two entities are bland cytologically and show a sharp interface with the surrounding pulmonary parenchyma, unlike BAC. Another point that was often raised in the older literature on BAC concerned the great difficulty with which metastases to the lung could be distinguished from the former neoplasm. Selected immunohistologic markers—especially nuclear labeling for thyroid transcription factor-1 (TTF-1; Fig. 16-31) and cytoplasmic staining for napsin-A—are valuable in distinguishing BAC from metastases of extrapulmonary ACAs,77–80 but that separation must ultimately rest on careful analysis of conventional clinicopathologic data.
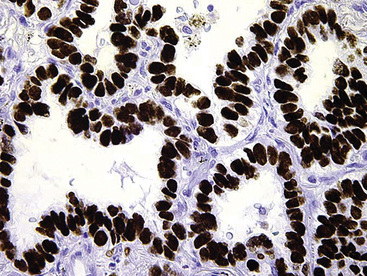
Figure 16-31 Intense nuclear immunoreactivity for thyroid transcription factor-1 is present in this bronchioloalveolar carcinoma.
Prognostically, patients with multifocal or pseudopneumonic BACs have an outlook that is worse than that of patients with unicentric tumors of this type because many of the former lesions are inoperable. Furthermore, mucinous tumors tend to behave more aggressively—with a higher incidence of extrapulmonary metastasis—than nonmucinous BAC when they are matched by size and stage.57,58 Overall, nonmucinous tumors measuring less than 3 cm in maximum dimension have a good prognosis, approximating 90% at 5 years. Indeed, the current surgical approach to such lesions is limited resection, principally by wedge excision (Fig. 16-32).81–85
The natural history of BAC is more protracted than that of more conventional pulmonary ACAs, and tumor-related fatalities will continue to accrue even at 10 years after diagnosis.57,63 Nevertheless, in an often-cited study by Manning and colleagues,62 the 5-year survival rate for nonmucinous BAC was 72%, whereas only 26% of patients with mucinous tumors survived at that point.
Atypical Adenomatous Hyperplasia and Its Relationship to Bronchioloalveolar Carcinoma
Kitamura and colleagues86 addressed the conceptual mechanistic relationship between topographically small atypical glandular proliferations of the lung—“atypical adenomatous hyperplasia” (AAH)—and BAC. Their model appeared to demonstrate a stepwise progression from AAH to BAC, with further evolution to invasive growth. That concept also had been advanced before, especially by Miller and colleagues,87 who postulated that such a stepwise process existed in the lung in analogy to the adenoma-carcinoma sequence in the colon.
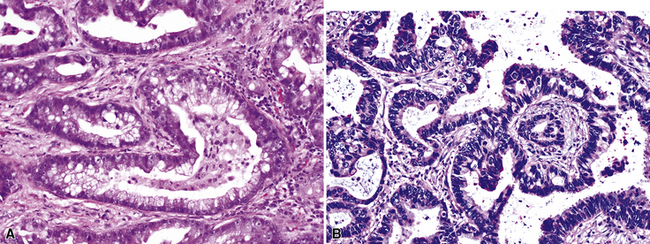
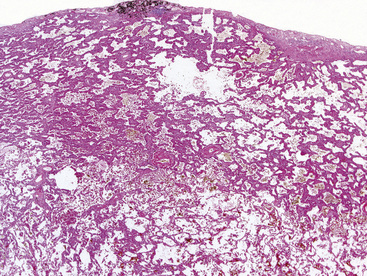
Atypical adenomatous hyperplasia must be differentiated from reactive or regenerative pneumocytic lesions, at one end of the spectrum, and from small bona fide ACAs, at the other. With regard to separation of AAH from various reactive lesions, Kitamura and co-workers86 have emphasized the tendency of reactive lesions to include multiple cell types, including type II pneumocytes, ciliated cells, and mucinous cells, and they have described the relatively more conspicuous interstitial inflammation and edema in localized interstitial pneumonitis. Additional criteria that are found to be helpful in this context involve assessment of the lesional borders and patterns of fibrosis. There is a tendency for lesions of AAH to be more sharply circumscribed and for the mild interstitial fibrosis and inflammation to stop at the same boundary as the atypical alveolar cells. Conversely, reactive lesions tend to be less well defined, and the interstitial scarring extends beyond the areas of alveolar cell atypia. The individual cells in AAH, although less homogeneous than those in BAC, also tend to be more uniformly atypical than those of reactive hyperplasias (Figs. 16-33 and 16-34).
Gupta and colleagues88 identified factors that favored the diagnosis of BAC over reactive changes in an evidence-based construct: multiple growth patterns; anisocytosis; nuclear atypia in 75% or more of the lesional cells; macronucleoli; and atypical mitoses. Conflicting information has emerged on the use of p63 immunostains to make this diagnostic distinction. Sheikh and colleagues89 suggested that p63 positivity was restricted to reactive processes and absent in nonmucinous BAC, whereas Saad and coworkers90 found p63 reactivity in 89% of cases of BAC.
A variety of chemotherapeutic agents can induce striking degrees of cytologic atypia, and this phenomenon is a well-documented pitfall in exfoliative cytology.74,91 We have also seen several examples of pneumocytes with intranuclear cytoplasmic inclusions in clear-cut cases of organizing phase diffuse alveolar damage; hence, their presence should not be viewed as pathognomonic of neoplasia.
It is our view that the distinction between AAH and small nonmucinous BAC is conceptually arbitrary. Standard criteria that have been cited as useful in this distinction include uniformly atypical nuclei, large lesional size (>5 mm), and complex growth, with budding or tufting of tumor cells in the alveolar spaces in BAC but not AAH.75,92 Kitamura and coworkers86 suggested that a nuclear area of less than 40 μm2 and a lesional diameter of less than 5 mm could effectively identify AAH as opposed to small BAC. Miller93 also proposed a limit of 5 mm to separate “bronchioloalveolar cell adenoma” from BAC.
Nevertheless, morphometric and immunohistologic analyses have shown a synonymity rather than a disparity between AAH and nonmucinous BAC.94,95 Similarly, molecular studies, which show some differences in statistical groups, have demonstrated many more shared features than differences.96–100
In light of the current availability of biologic agents that can be used to treat lung cancer, it is appropriate to mention the genotypes of nonmucinous and mucinous BAC. In general, nonmucinous lesions demonstrate mutations in the epidermal growth factor receptor (EGFR) molecule, to which tyrosine kinase inhibitor (TKI) therapeutic agents are directed.101,102 On the other hand, mucinous BAC manifests preferential aberrations in the K-ras gene and accordingly does not show a response to TKIs.101 Mutant EGFR protein overexpression, as indicated indirectly by strong cell membrane immunoreactivity in tumor cells, correlates to some degree, but very imperfectly, with in situ hybridization studies or polymerase chain reaction-based assays.103
“Micropapillary” ACA of the lung was formerly considered by many observers to be a subtype of nonmucinous BAC. That nosologic approach has now changed,43 occasioned by the demonstrably worse prognosis of micropapillary carcinoma.104,105 Accordingly, the latter neoplasm is now regarded as a pathologic entity unto itself. In analogy to the diagnostic approach to BAC, a conclusive interpretation of micropapillary carcinoma should be avoided in cytologic specimens. Rudomina and colleagues106 have shown that papillary profiles in the latter samples do not correlate well with a final diagnosis of micropapillary ACA.
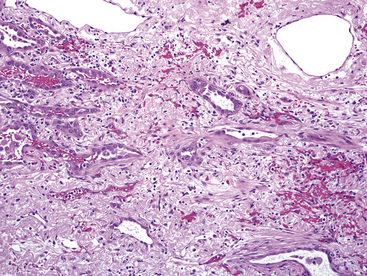
Adenocarcinomas Associated with Scars
In the relatively recent past, it was taught that fibrous scarring in the lung—seen as a consequence of pneumonia, interstitial fibroproliferative diseases, or pneumoconioses—predisposed to ACA and had a directly causative role in the genesis of that tumor type.107 Nevertheless, several investigators have concluded that the central fibrosis seen in “scar adenocarcinomas” (Fig. 16-35) is formed after initiation of the carcinoma and that it is the product of the tumor cells themselves.108–110 At a practical level, there is no reason to suspect that localized fibrosing conditions in the lung are, in and of themselves, preneoplastic. However, it appears that an increased frequency of lung carcinoma may exist in patients with diffuse interstitial fibrosis—as seen in late-stage “usual interstitial pneumonia,” for example—over and above that associated with smoking alone.111 Nevertheless, the relative weights of those potentially causal elements are still unclear.
With particular reference to asbestosis and silicosis, special forms of pulmonary interstitial fibrosis, our review of the aggregated literature leads to the conclusion that the risk of pulmonary carcinoma may (debatably) be increased by those conditions of the lung, although such an association does not prove causation. It is clear that cigarette smoking is, by far, the most significant carcinogenic factor in this specific context.112
Adenosquamous Carcinoma
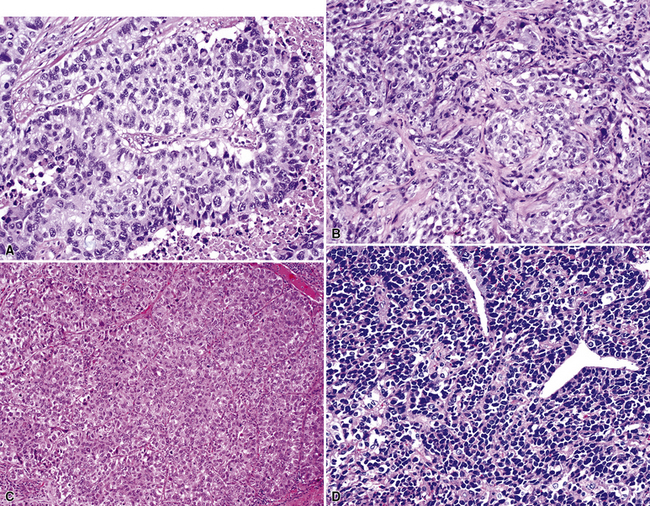
Adenosquamous carcinoma (ASC) is a “composite” tumor, exhibiting simultaneous squamous and glandular differentiation in the same mass (Fig. 16-36). It accounts for no more than 5% of all lung cancers in most surgical series.113–115 The clinical, radiographic, and gross pathologic attributes of ASC are most similar to those of “pure” ACAs of the lung. A point of contention with regard to this lesion is whether it is synonymous with high-grade mucoepidermoid carcinoma of the salivary glandular type. Our opinion is that those two neoplasms are typically separable. Salivary gland analog tumors in the lung, as considered subsequently, tend to arise in the large central airways, in contrast to the propensity for ASC to be peripheral. In addition, foci of lower-grade mucoepidermoid carcinoma are often present in the former, but not the latter, of these tumor types. The prognosis of pulmonary ASC is said to be adverse. In studies reported by Ishida and colleagues,113 Takamori and colleagues,115 and Cakir and co-workers,116 the survival of patients with adenosquamous tumors was statistically worse than that of individuals with “pure” ACAs or SCCs.
Large Cell Carcinoma
Large cell undifferentiated carcinomas account for approximately 15% of all lung cancers.117 As mentioned earlier, diagnostic use of the term “non–small cell carcinoma” has produced some confusion among poorly differentiated SCC, poorly differentiated ACA, poorly differentiated ASC, and true LCC. Accordingly, it has been suggested that the designation of “large cell carcinoma” should be employed restrictively as a synonym for LCC. An even more extreme point of view is that current pathologic tools for cellular analysis have made this diagnosis completely obsolete.118,119
Large cell carcinomas are typically larger than 5 cm in maximum dimension, have a white-gray cut surface (which may be lobulated and resemble “fish flesh,” thus potentially simulating the appearance of a sarcoma or a hematolymphoid lesion; Fig. 16-37), and are rarely multicentric. Internal necrosis is a relatively common feature. Approximately 50% demonstrate a connection to a large tubular airway.
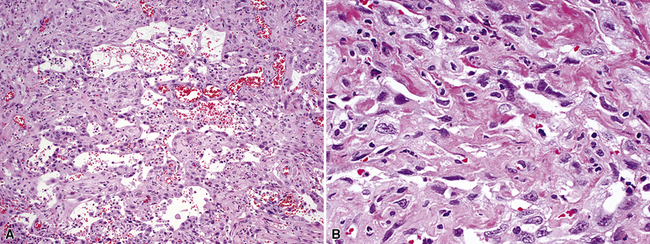
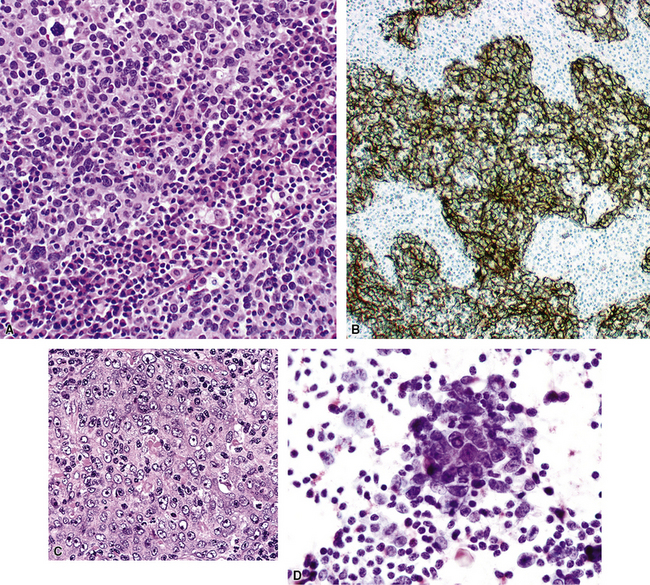
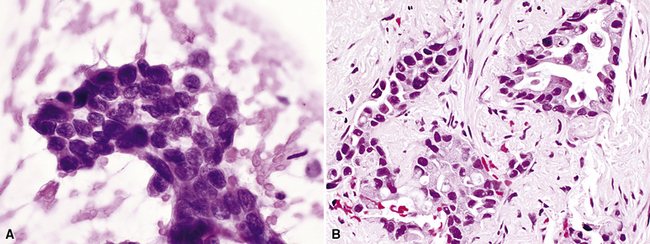
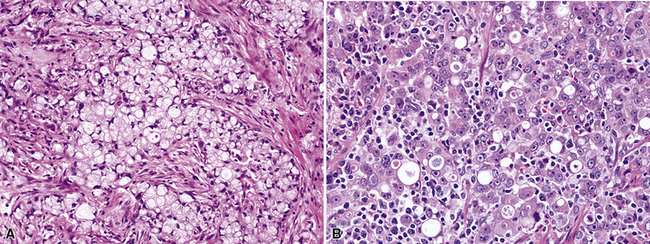
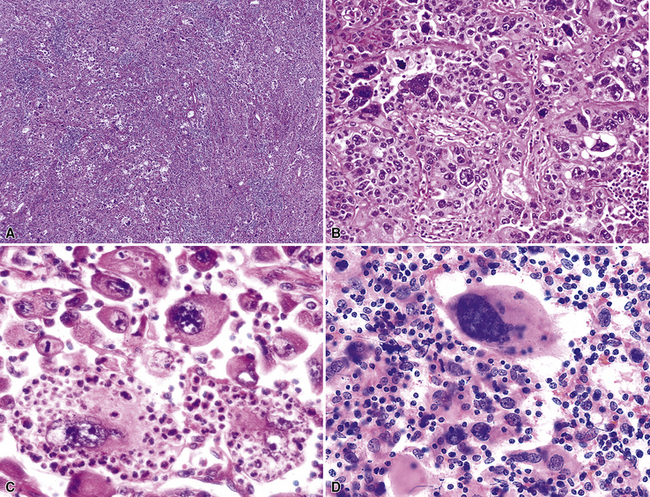
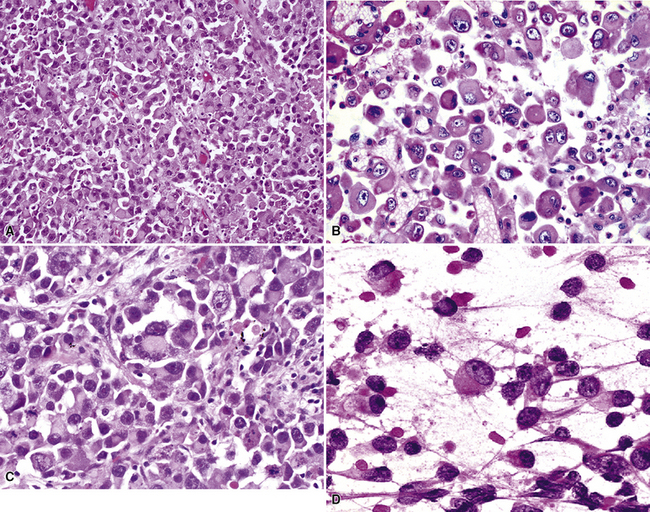
Histologically, LCCs show a composition of large polygonal cells with vesicular chromatin, prominent nucleoli, discernible cytoplasmic borders, and by definition, a lack of glandular differentiation or keratinization (Fig. 16-38). They are typically arranged in sheets or large clusters, potentially exhibiting foci of central necrosis. Two distinctive subtypes also exist—giant cell carcinoma and clear cell carcinoma.
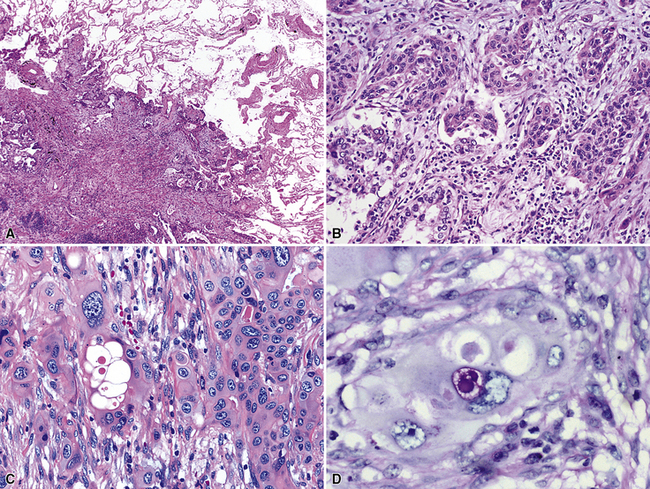
Giant cell carcinoma was initially believed to be a separate clinicopathologic entity,120,121 but that philosophy is no longer considered valid.122 Microscopically, this variant of LCC is composed of extremely pleomorphic large tumor cells, which are often multinucleated (Fig. 16-39). There is a regular admixture of polymorphonuclear leukocytes with the neoplastic elements, even in the absence of necrosis, suggesting tumoral synthesis of leukocyte cytokines, such as granulocyte colony–stimulating factor.123 Parenthetically, this phenomenon can also be associated with systemic neutrophilia in association with the giant cell subtype of LCC. Neoplastic “cannibalism” may also be observed, wherein the giant tumor cells appear to engulf one another. One subtype of pulmonary giant cell carcinoma bears a close resemblance to choriocarcinoma of the gonads, complete with tumor synthesis of beta-human chorionic gonadotropin.124
Primary clear cell carcinoma of the lung (CCCL) is a diagnosis of exclusion, and it is likely that tumors with both squamous and glandular differentiation are included in that group. A number of other clear cell neoplasms of the lung, including some “carcinoids,” the benign “sugar tumor,” metastatic renal cell carcinoma, and metastatic “balloon cell” melanoma, must also be considered before making the diagnosis of CCCL.50,125–129 This can be accomplished by a combination of radiographic, electron microscopic, and immunohistologic evaluations. The overall clinicopathologic attributes of CCCL are comparable to those of LCC, not otherwise specified.
In the last two decades, it has been suggested that a subset of pulmonary large cell carcinomas that show occult neuroendocrine differentiation—as detected only by electron microscopy or immunohistology—should be nosologically separated from truly undifferentiated large cell tumors.130–133 Hence, the terms “exocrine large cell carcinoma” (another synonym for LCC) and “endocrine large cell carcinoma” have entered use.132 In our opinion, “endocrine large cell carcinomas” are best specified as either high-grade “pure” neuroendocrine carcinomas, large cell type, or LCCs with occult neuroendocrine differentiation; those two entities are considered in more detail in another chapter on neuroendocrine neoplasms of the lung (see Chapter 13).
Selected large cell lung cancers have a “rhabdoid” phenotype134 with eosinophilic hyaline inclusions in the cytoplasm and large vesicular nuclei with prominent nucleoli (Fig. 16-40). It is likely that this image represents a final common pathway of clonal evolution (“dedifferentiation”) in carcinomas of the lung, as in several other neoplasms demonstrating a rhabdoid configuration.135 That conclusion is supported by the fact that other forms of carcinoma may be admixed with the rhabdoid elements (“composite” extrarenal rhabdoid tumors).135 Moreover, nuclear expression of the INI1 gene—a tumor suppressor—is retained in “composite” extrarenal rhabdoid tumors (Fig. 16-41), but is consistently deleted in prototypical rhabdoid tumor of the kidney in children.136–138