We sought to determine the intravascular ultrasound-derived anatomic criteria for functionally significant lesions in small coronary arteries with a reference segment diameter <3 mm. A fractional flow reserve (FFR) of <0.75, as determined by pressure wire using high-dose (100 to 150 μg) intracoronary adenosine, was used as the reference standard for functional significance. For the 94 patients/lesions involved in the present study, the average reference vessel diameter was 2.72 mm. The FFR was <0.75 in 38 patients (40.4%) and ≥0.75 in 56 patients (59.6%). Logistic regression analysis identified the minimal lumen area, plaque burden, and lesion length as the 3 most important determinants of the FFR. Using classification and regression tree analysis, the best cutoff values for these determinants to discriminate a FFR of <0.75 versus ≥0.75 were a minimal lumen area of ≤2.0 mm 2 (sensitivity 82.35%, specificity 80.77%), plaque burden of ≥80% (sensitivity 87.9%, specificity 78.9%), and lesion length of ≥20 mm (sensitivity 63.6%, specificity 78.9%). A significant increase was found in the area under the receiver operating characteristic curve of the combined parameters (minimal lumen area plus plaque burden plus lesion length) compared to the plaque burden (p = 0.014) and other individual parameters (p <0.001). In conclusion, we found that intravascular ultrasound-derived anatomic criteria are able to predict the functional significance of intermediate lesions in small coronary arteries. A minimal lumen area of ≤2.0 mm 2 , plaque burden of ≥80%, and lesion length of ≥20 mm predicted a FFR of <0.75 with good sensitivity and specificity.
The determination of the functional significance of intermediate coronary lesions is crucial but has remained problematic. Visual interpretation of lesion severity on coronary angiography, even with quantitative coronary angiography, correlates poorly with functional significance. Noninvasive stress tests before diagnostic coronary angiography are often not performed, and the results are sometimes inconclusive. To date, intravascular ultrasound (IVUS) scans and pressure wire are 2 techniques that have been useful. Compared to pressure wire, IVUS scans have the additional advantages of being able to guide the selection of the balloon and stent size, assess stent expansion and apposition, and uncover stent edge dissection and residual stenosis. Previous studies suggested that the minimal lumen area (MLA), as determined using IVUS scanning, correlated with coronary physiology, and a MLA of <4 mm 2 was found to be the threshold for flow-limiting stenosis in most studies. However, this criterion is only applicable to lesions located at a proximal segment of non–small coronary arteries with a reference segment diameter >3 mm, limiting the use of IVUS-derived anatomic criteria to define the functional significance of a subset of lesions. Currently, no relevant data are available for small coronary arteries, which are particularly common in Asian patients. We hypothesized that the corresponding IVUS-derived anatomic criteria for functional significance would be different in small coronary arteries with a reference segment diameter of <3 mm.
Methods
The Intravascular ultrasound Diagnostic Evaluation of Atherosclerosis in Singapore (IDEAS) study was a prospective study conducted at 2 centers in Singapore. We sought to determine the IVUS-derived anatomic threshold for functionally significant lesions in small coronary arteries. In the present study, a fractional flow reserve (FFR) of <0.75, as determined by pressure wire (Certis, Radi Medical, Uppsala, Sweden) after high-dose intracoronary adenosine, was used as the reference standard for functional significance. Patients aged 21 to 80 years who had undergone nonurgent coronary angiography and were found to have at least one intermediate de novo lesion (30% to 75% stenosis, visual estimation) in a small native coronary artery (reference segment diameter <3.0 mm, visual estimation) were suitable for recruitment. The exclusion criteria for the present study were unstable coronary syndrome with continuous chest pain and/or hypotension (systolic blood pressure <90 mm Hg), unable to give informed consent, significant bradycardia (<50 beats/min) without a pacemaker in situ, myocardial infarction (recent or old) in the territory of the study lesion, previous intervention treatment to the target vessel, an ostial lesion, a thrombus-laden lesion, a left main lesion, and another lesion >20% in the target coronary artery. The demographic and clinical characteristics were collected prospectively by a dedicated research nurse. The IDEAS study complied with the Declaration of Helsinki, in that the locally appointed ethics committee approved the research protocol and all subjects (or their guardians) provided informed consent.
A 6Fr guiding catheter (without side hole) was used to selectively cannulate the ostium of the target coronary artery. All angiographic images captured were analyzed, and off-line quantitative coronary angiography (CAAS, Pie Medical Imaging, Maastricht, The Netherlands) was performed by an experienced angiographer, who was unaware of the results of the FFR determination and IVUS examination. The minimal lumen diameter, reference segment diameter, percentage of diameter stenosis, and lesion length were measured using standard techniques.
Unfractionated heparin (3,000 IU) was administered first. A guiding shot was taken after intracoronary nitroglycerin (200 μg) had been administered through the guiding catheter. A 0.014-in. pressure wire (Certiu, Radi) was advanced through the guiding catheter. “Zeroing” was performed when the wire sensor was at the position of the guiding catheter tip. The pressure wire was then advanced across the stenotic segment, with the sensor ≥20 mm distal to the lesion. Intracoronary adenosine was used as the sole hyperemic stimulating agent. To evaluate intermediate lesions in any of the 3 coronary arteries, adenosine (100 μg) was administered through the guiding catheter. A total of 3 cycles of measurement was performed, and the lowest FFR was chosen as the final result. A higher dose of adenosine (150 μg) was used when the FFR was 0.75 to 0.80. The lesion was considered functionally significant when the FFR was <0.75.
Immediately after the FFR was measured, but before balloon predilation, IVUS interrogation was performed using a 40-MHz Atlantis SR IVUS catheter (Boston Scientific, Natick, Massachusetts). IVUS imaging was acquired and stored during the motorized pullback (0.5 mm/s) of the imaging catheter. The IVUS images were recorded on CD-ROM for blinded off-line quantitative analysis. Off-line analysis was performed with a commercially available program for computerized planimetry (EchoPlaque, INDEC System, Mountain View, California). The lesion site selected for the analyses was the image slice with the smallest lumen cross-sectional area. The proximal and distal reference segments were the most normal-appearing cross-sections within 10 mm proximal or distal to the lesion but before any major side branch. The following parameters were measured at the lesion site: (1) minimal lumen diameter, (2) MLA, (3) percentage of area stenosis (100 × [average reference lumen area − lesion lumen area]/average reference lumen area), (4) plaque burden, (5) lesion length, and (6) remodeling index (100 × external elastic membrane at lesion/average external elastic membrane area at proximal and distal reference segment). Positive remodeling was defined as a remodeling index >1 and absent/negative remodeling as a remodeling index of ≤1.
Data on the 30-day clinical outcomes of the patients were obtained by telephone interview and/or case note review by a dedicated research nurse. The clinical end points included death, myocardial infarction, and target vessel revascularization.
The association between FFR (categorized as <0.75 vs ≥0.75) to the angiographic and IVUS parameters were evaluated using the chi-square test and logistic regression analysis. The area under the receiver operating characteristic curve was also estimated for each significant predictor of the logistic model individually and jointly. Classification and regression tree analysis was also performed to identify the significant risk factors for a low FFR and their cutoffs. The κ statistic was used to evaluate the agreement of lesion significance between the FFR measurement and visual interpretation of the angiographic images, as reviewed by the 2 interventional cardiologists. Statistical analyses were primarily generated using Stata, version 10 (StataCorp, College Station, Texas), assuming a 2-sided test at the 5% significance level.
Results
A total of 94 patients (94 lesions) were recruited into the IDEAS study from August 2007 to July 2009. The ethnic composition of the recruited patients was Chinese (n = 63, 67%), Malaysian (n = 19, 20.2%), and Indian (n = 9, 9.6%), in accordance with the ethnic composition of Singapore. The mean body height and weight was 1.65 ± 0.07 m and 70.0 ± 11.7 kg, respectively, with a median body mass index of 25 kg/m 2 (range 17 to 38). The demographic and clinical characteristics of the study population are listed in Table 1 . More than 40% of the recruited patients had diabetes mellitus. The most common indication for coronary angiography was stable chest pain. In patients undergoing coronary angiography for non–ST-segment elevation myocardial infarction, all the study lesions were the nonculprit lesion for the myocardial infarction. None of the patients had undergone noninvasive stress tests before the procedure.
| Characteristic | All (n = 94) | FFR | p Value | |
|---|---|---|---|---|
| <0.75 (n = 38) | ≥0.75 (n = 56) | |||
| Age (years) | 0.003 | |||
| Median | 58 | 52 | 60 | |
| Range | 35–83 | 41–75 | 35–83 | |
| Gender | 0.797 | |||
| Men | 73 (77.7%) | 29 (76.3%) | 44 (78.6%) | |
| Women | 21 (22.3%) | 9 (23.7%) | 12 (21.4%) | |
| Ethnicity | 0.962 | |||
| Chinese | 63 (67.0%) | 26 (41.3%) | 37 (58.7%) | |
| Malaysian | 19 (20.2%) | 8 (42.1%) | 11 (57.9%) | |
| Indian | 9 (9.6%) | 3 (33.3%) | 6 (66.7%) | |
| Other | 3 (0.03%) | 1 (0.03%) | 2 (0.04%) | |
| Mean height (m) | 1.65 (0.07) | 1.64 (0.07) | 1.65 (0.07) | 0.441 |
| Mean weight (kg) | 70.1 (11.7) | 68.0 (10.6) | 71.5 (12.2) | 0.078 |
| Body mass index (kg/m 2 ) | 0.212 | |||
| Median | 25 | 24 | 26 | |
| Range | 17–38 | 18–38 | 17–38 | |
| Smoking | 34 (36.2%) | 10 (26.3%) | 24 (42.9%) | 0.101 |
| Diabetes mellitus | 38 (40.4%) | 17 (44.7%) | 21 (37.5%) | 0.178 |
| Hypertension | 61 (64.5%) | 22 (57.9%) | 39 (69.6%) | 0.242 |
| Hyperlipidemia ⁎ | 78 (83.0%) | 33 (86.8%) | 45 (80.4%) | 0.412 |
| Family history of coronary artery disease | 11 (11.7%) | 6 (15.8%) | 5 (8.9%) | 0.310 |
| Previous myocardial infarction | 17 (18.1%) | 12 (31.6%) | 5 (0.1%) | 0.005 |
| Indication | ||||
| Stable chest pain | 74 (78.7%) | 29 (76.3%) | 45 (80.4%) | 0.638 |
| Unstable angina | 2 (2.1%) | 2 (5.3%) | 0 (0.0%) | 0.083 |
| Non–ST-segment elevation myocardial infarction | 18 (19.2%) | 7 (18.4%) | 11 (19.6%) | 0.883 |
⁎ Defined as a previous diagnosis by a physician, the use of lipid-lowering drugs, a total cholesterol level of ≥240 mg/dl, or a serum triglyceride concentration of ≥135 mg/dl.
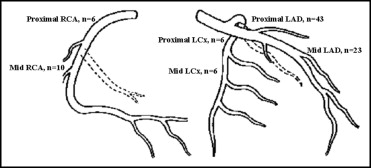
The study vessel and lesion location are shown in Figure 1 . The left anterior descending artery was the most common study vessel. More than 1/2 of the lesions were located at the proximal vessel segment. Off-line quantitative coronary angiography was performed for all study lesions ( Table 2 ). The average reference vessel diameter was 2.72 mm. Diameter stenosis was 30% to 75% in 85 patients (90.4%).
| Variable | All (n = 94) | FFR | Crude OR (95% CI) | p Value | |
|---|---|---|---|---|---|
| <0.75(n = 38) | ≥0.75(n = 56) | ||||
| Angiographic parameters | |||||
| Reference segment diameter (mm) | 2.72 ± 0.3 | 2.7 ± 0.3 | 2.8 ± 0.3 | 0.32 (0.08–1.24) | 0.101 |
| Minimal lumen diameter (mm) | 1.3 ± 0.4 | 1.0 ± 0.3 | 1.4 ± 0.4 | 0.05 (0.01–0.24) | <0.001 |
| Percentage of diameter stenosis | 54.1 ± 14.0 | 61.2 ± 12.3 | 49.3 ± 13.1 | 1.08 (1.04–1.12) | <0.001 |
| Lesion length (mm) | 15.1 ± 6.0 | 18.0 ± 5.9 | 13.2 ± 5.3 | 1.17 (1.07–1.28) | <0.001 |
| Intravascular ultrasound parameters | |||||
| Proximal reference segment | |||||
| External elastic membrane area (mm 2 ) | 12.1 ± 3.2 | 12.3 ± 2.6 | 11.9 ± 3.6 | 1.04 (0.90–1.19) | 0.613 |
| Lumen area (mm 2 ) | 5.5 ± 1.8 | 5.0 ± 1.5 | 5.7 ± 1.9 | 0.78 (0.60–1.02) | 0.072 |
| Lesion | |||||
| External elastic membrane area (mm 2 ) | 10.2 ± 3.1 | 10.7 ± 2.7 | 9.9 ± 3.3 | 1.09 (0.95–1.26) | 0.228 |
| Minimum lumen area (mm 2 ) | 2.3 ± 1.0 | 1.7 ± 0.3 | 2.6 ± 1.1 | 0.03 (0.01–0.15) | <0.001 |
| Minimum lumen diameter (mm) | 1.5 ± 0.3 | 1.4 ± 0.1 | 1.6 ± 0.3 | 0.001 (0–0.011) | <0.001 |
| Lesion plaque burden (%) | 77.1 ± 9.6% | 83.6 ± 4.3% | 72.9 ± 9.8% | 1.26 (1.13–1.41) | <0.001 |
| Lesion length (mm) | 17.9 ± 8.1 | 22.4 ± 8.7 | 15.1 ± 6.3 | 1.15 (1.07–1.24) | <0.001 |
| Distal reference segment | |||||
| External elastic membrane area (mm 2 ) | 10.6 ± 4.0 | 9.4 ± 2.9 | 11.3 ± 4.4 | 0.87 (0.76–0.99) | 0.032 |
| Lumen area (mm 2 ) | 5.9 ± 2.2 | 5.3 ± 1.6 | 6.3 ± 2.5 | 0.80 (0.65–0.99) | 0.047 |
| Remodeling index >1 | 31 (33.3%) | 19 (51.4%) | 12 (21.4%) | 3.9 (1.6–9.6) | 0.003 |
| Area stenosis | 37.6% (20.1–85.7) | 31.6% (20.1–50.6) | 43.7% (24.9–85.7) | 0.91 (0.86–0.96) | <0.001 |
The pressure wire was inserted across the lesions, and the FFR was measured successfully in all 94 recruited patients. No pressure wire-related complications occurred. Intracoronary adenosine was used as the hyperemic stimuli in all patients. The maximum dose of adenosine administered was 100 μg in 88 patients and 150 μg in 6 patients. Ventricular fibrillation, promptly reverted using an external defibrillator, occurred in 1 patient during the administration of intracoronary adenosine (100 μg) to the right coronary artery. After defibrillation, repeated administration of adenosine was uneventful in this patient. No significant adenosine-induced bradycardia requiring temporary pacing developed.
The overall median FFR was 0.81 (range 0.41 to 1.00). When categorized according to functional significance, the FFR was <0.75 in 38 patients (40.4%) and ≥0.75 in 56 patients (59.6%). In the FFR <0.75 group, the median FFR was 0.67 (range 0.41 to 0.74); in the FFR ≥0.75 group, the median FFR was 0.86 (range 0.75 to 1.00). The demographic and clinical characteristics of the patients in the FFR <0.75 and ≥0.75 groups are listed in Table 1 . The patients in the FFR <0.75 group were significantly younger and more likely to have had previous myocardial infarction.
Of the 94 patients, IVUS pullback images were available for off-line quantitative analysis for 86 patients (91.5%). Of the 8 excluded patients, the IVUS catheter was unable to be inserted across the lesion because of calcification and/or tortuosity in 5 patients (FFR <0.75, n = 3; FFR ≥0.75, n = 2). The IVUS images were suboptimal for analysis in 1 patient and were not recorded for 2 patients because of machine failure (n = 1) and technical mistakes (n = 1). No IVUS-related complications occurred.
The logistic regression analysis identified MLA, plaque burden, and lesion length to be the 3 most important determinants of FFR ( Table 3 ). The areas under the receiver operating characteristic curves for the different IVUS parameters are listed in Table 4 . These data suggested that individually, the plaque burden, followed by MLA and lesion length were the 3 strongest predictors of FFR with a receiver operating characteristic of 0.87 (95% confidence interval [CI] 0.79 to 0.95), 0.87 (95% CI 0.79 to 0.94), and 0.75 (95% CI 0.64 to 0.86), respectively. A significant increase was seen in the receiver operating characteristic for the combined parameters (MLA plus plaque burden plus lesion length) compared to the plaque burden alone (0.014) and other individual IVUS parameters (p <0.001; Figure 2 ).



